It’s common to hear phrases like “that’s how I slipped a disc,” “doing that caused me to throw my back out,” and “lifting like that you’re going to blow a disc” in the gym.
These illustrate some of the existing fear-induced beliefs about the spine and lumbar flexion. For much of the last couple of decades, there has been a large push to ditch movements like sit-ups and transition to exercises like planks. Along with that, there has been an effort to educate people of the danger of lifting without a perfectly “neutral” back. This notion has extended out to the degree where some people will fear even the concept of picking up something as light as a piece of paper without maintaining a neutral spine. Although well meaning, the medical and fitness fields have contributed to and perpetuated this problem through an overly simplified narrative. Despite the strong convictions and assertive claims often made, the evidence is not quite as clear as people believe.
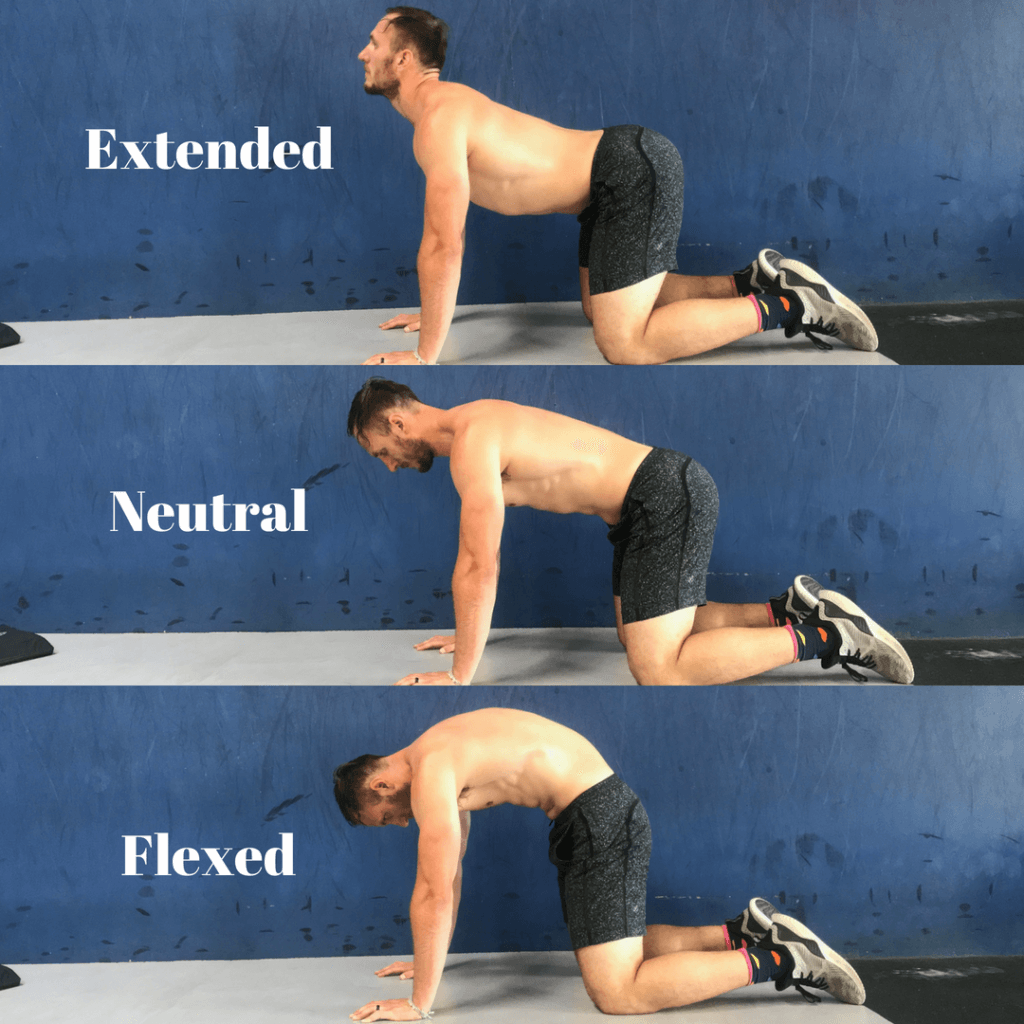
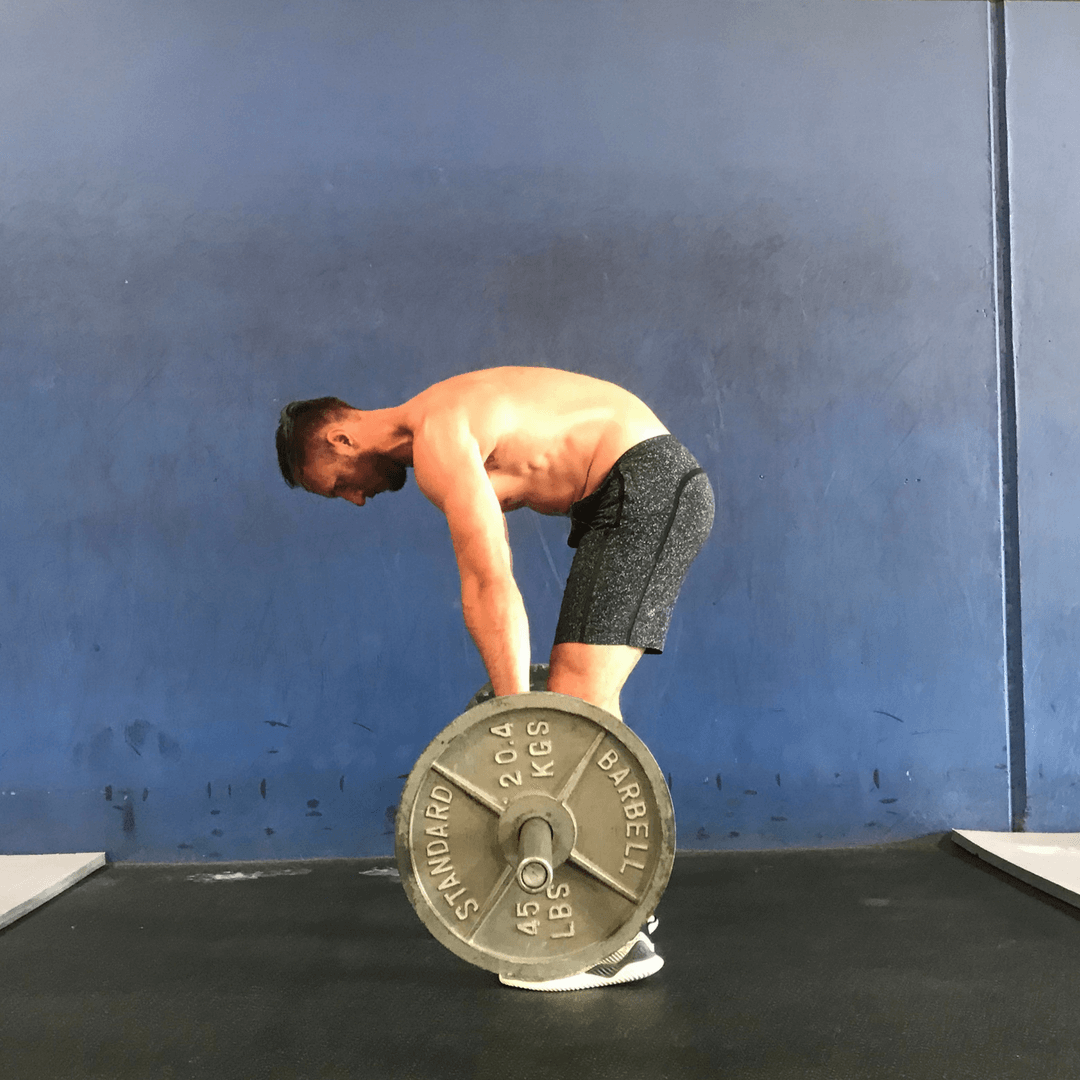
If you’ve spent much time in the world of rehabilitation or fitness, you’ve likely been drilled by the “neutral” spine concept. The concept of the neutral spine is that there is a specific position of the spine where it is safe from injury – particularly, from the dangers of lumbar flexion. Generally, when we discuss spinal flexion, there are two main types of activities that come up within the discussion: lifting with a flexed spine (i.e. deadlift/squat) and curling-type movements (i.e. sit-ups, leg raises). Most often, there is an argument against these for their increased risk of injury.
Digging into the literature, we come to a number of discussion points on this topic:
- What is neutral?
- Is lumbar flexion dangerous?
- Is lumbar flexion more dangerous than neutral?
- Is lumbar flexion better than neutral for anything?
First thing: A quick summary of some important anatomy and terminology for this topic.
Before we dive in, I’d like to thank Greg Lehman for inspiring this article. He was one of the first individuals to speak and write on this subject, and begin challenging status quo of flexion being inherently terrible. Check out his article where he discussed this topic as well.
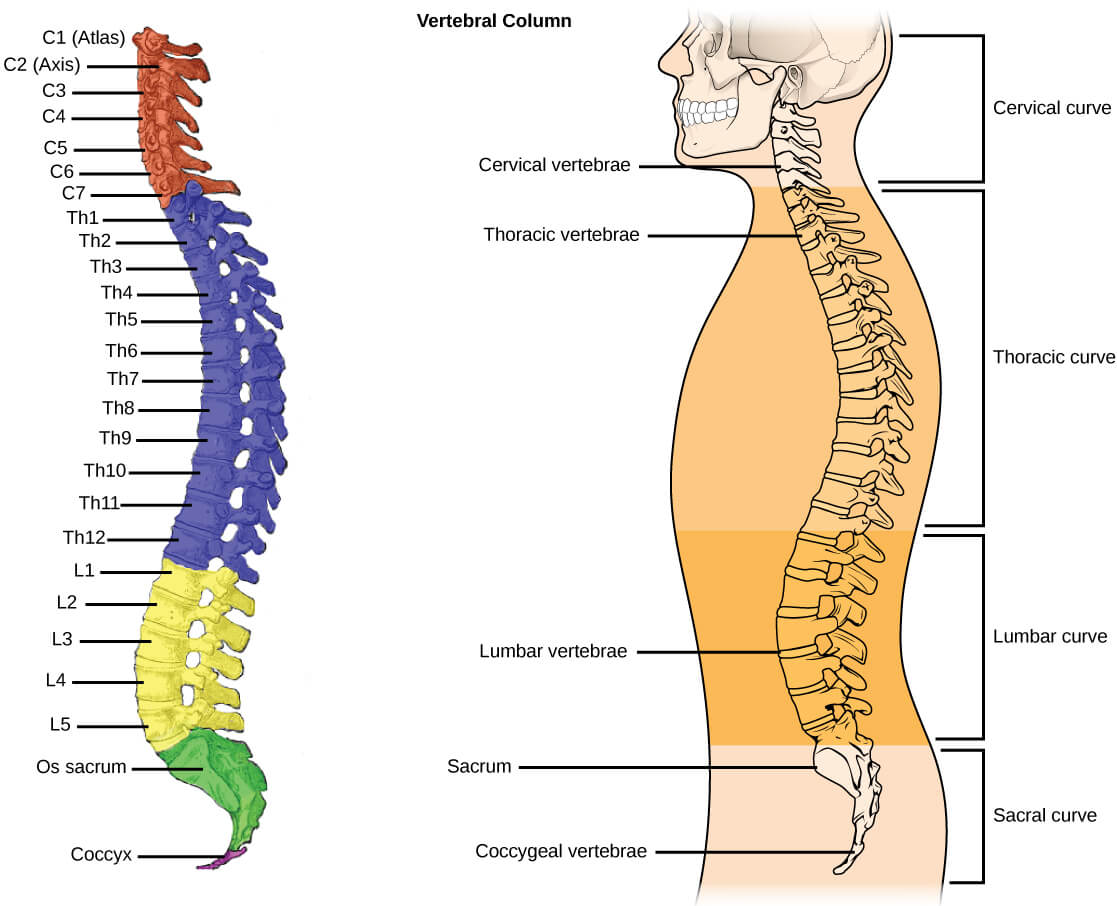
Anatomy
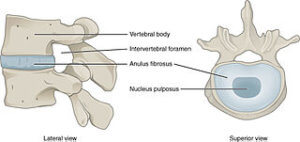
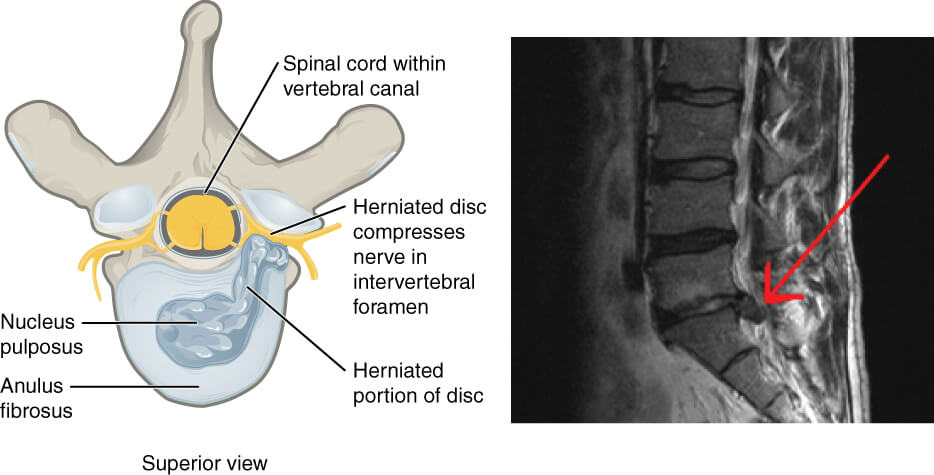
Between each spinal vertebrae is an intervertebral disc that helps to absorb shock and functions to dissipate and transfer load across segments. The disc is made up of a central nucleus pulposus, which is filled with a thick gel containing approximately 70-90% water and is surrounded by a series of annulus fibrosus. Each disc typically has 15-25 layers of annulus, which is made up of ~50% collagen and some elastin proteins. This structure helps to give a flexible but strong structure.
Each side of the disc has a vertebral endplate which acts as a means to connect the disc to the bone. When we are born, our end plates are thick and act as growth plates for the vertebrate, decreasing over time. The side of the end plate facing the disc is composed of mostly fibrocartilage, making it very strong; in contrast, the side facing the vertebrae is mostly composed of calcified cartilage, which makes it structurally weaker. It is generally considered to be the weakest segment of the region.
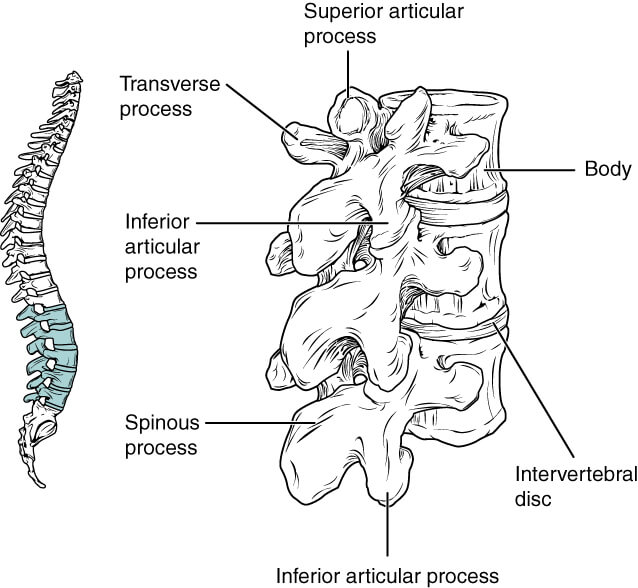
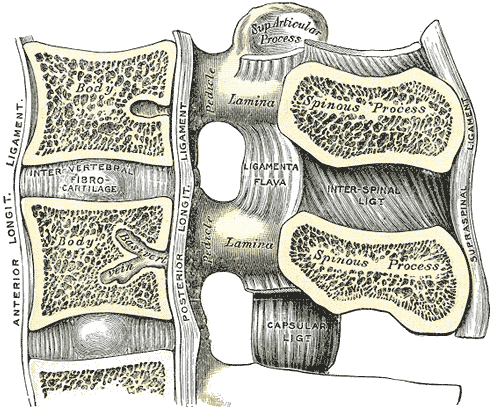
The lumbar spine is made up of five bony vertebrae with a disc between each segment. The vertebral column primarily functions to provide vertical stability to the torso, protect the spinal cord and nerve roots, and provide attachment points for musculature. Each vertebrae has a few major components: body, pedicle, lamina, spinous process, superior/inferior articular process, and transverse process.
Building on top of the bony structure, there is also a wide array of ligamentum support for the spinal column. There are ligament structures that span along multiple segments of the spine, such as the posterior longitudinal ligament and ligament structures that connect individual segments, such as the interspinous ligament. This diverse structure of ligaments helps to provide an incredibly high amount of passive support to the spine.
Spinal Motion
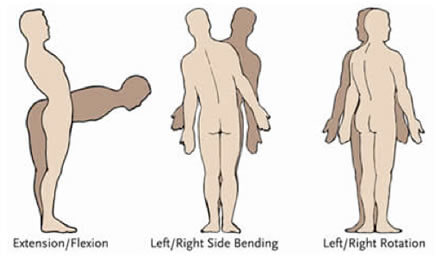
The lumbar spine can demonstrate four main types of motions: flexion, extension, rotation, and lateral flexion. This region generally shows 40-50° flexion, 15-20° extension, 5-7° rotation, and 20° lateral flexion. Lumbar flexion is generally limited due to soft tissue tension, whereas the other motions may be limited by either soft tissue tension or bony approximation. This is considered to be the global range of motion for the lumbar spine, with each segment having its own intervertebral range associated with it. Intervertebral range of motion varies by the segment, but it is generally representative of an equal distribution of the above ranges of motion.
Types of Pathologies
The lumbar spine has a range of pathologies that are associated with it, but we just want to touch on a few of the major ones related to this discussion.
A disc herniation is when the disc begins to push outward beyond its normal confines between the vertebrae. There are various kinds of herniation classifications, some of which are focused on the nucleus pulposus, others on the whole unit. Most commonly, a disc herniation will occur posterior or posterior-lateral toward neural tissue, but it can occur in any direction.
An endplate fracture is where there is disruption of the endplate, generally on the aspect of the endplate-bone interface. When an endplate fractures, it can allow for the nucleus pulposus to leak and become disrupted. The disc can become weakened through this and is then more likely to herniate.
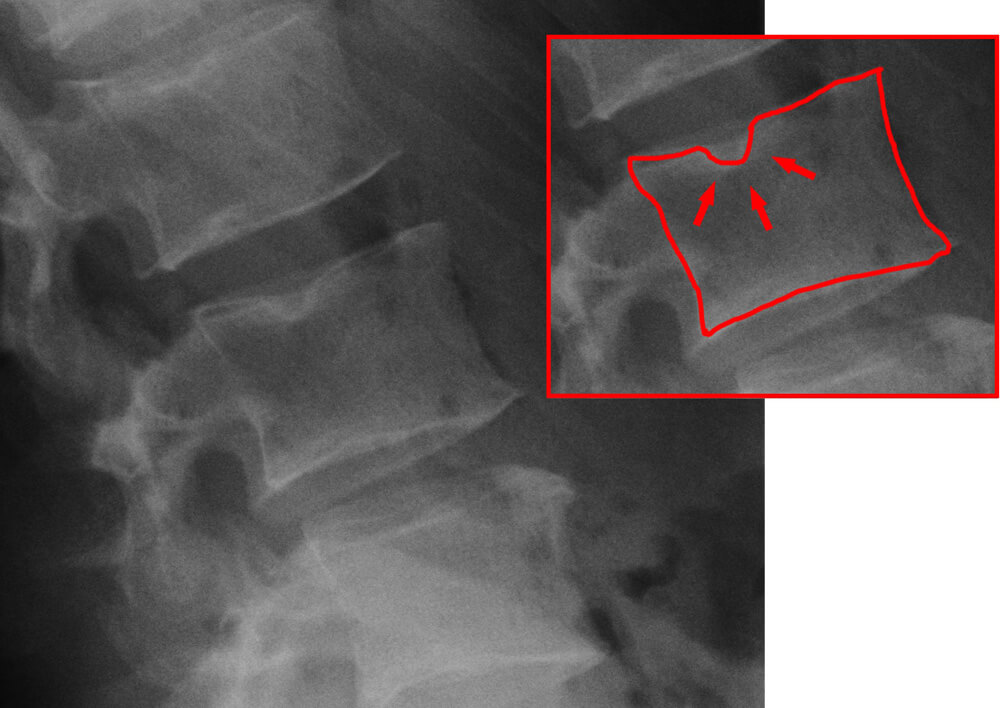
A spondylolysis is where damage occurs to the pars interarticularis (in essence a fracture). This has been found to occur in normal aging (with many of these occurring before the age of 2). A spondylolysis can progress to a spondylolisthesis, in which the vertebral body slides forward/backward (respectively to the segment you reference).
Now that we’ve cleared up the background details, let’s get back to the discussion at hand!
What is Neutral?
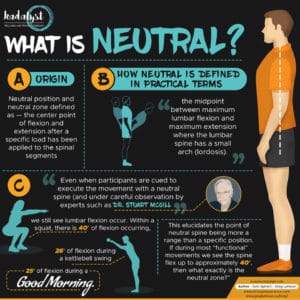
There are many terms that are often utilized in our field without a second thought. “Neutral spine” is probably one of the most used of these words. Should you ask a range of professionals to define neutral spine and explain why it matters, you’d likely receive a range of answers. This lack of consistent terminology between clinicians, researchers, and the public leaves room for miscommunication and greater error in information sharing.
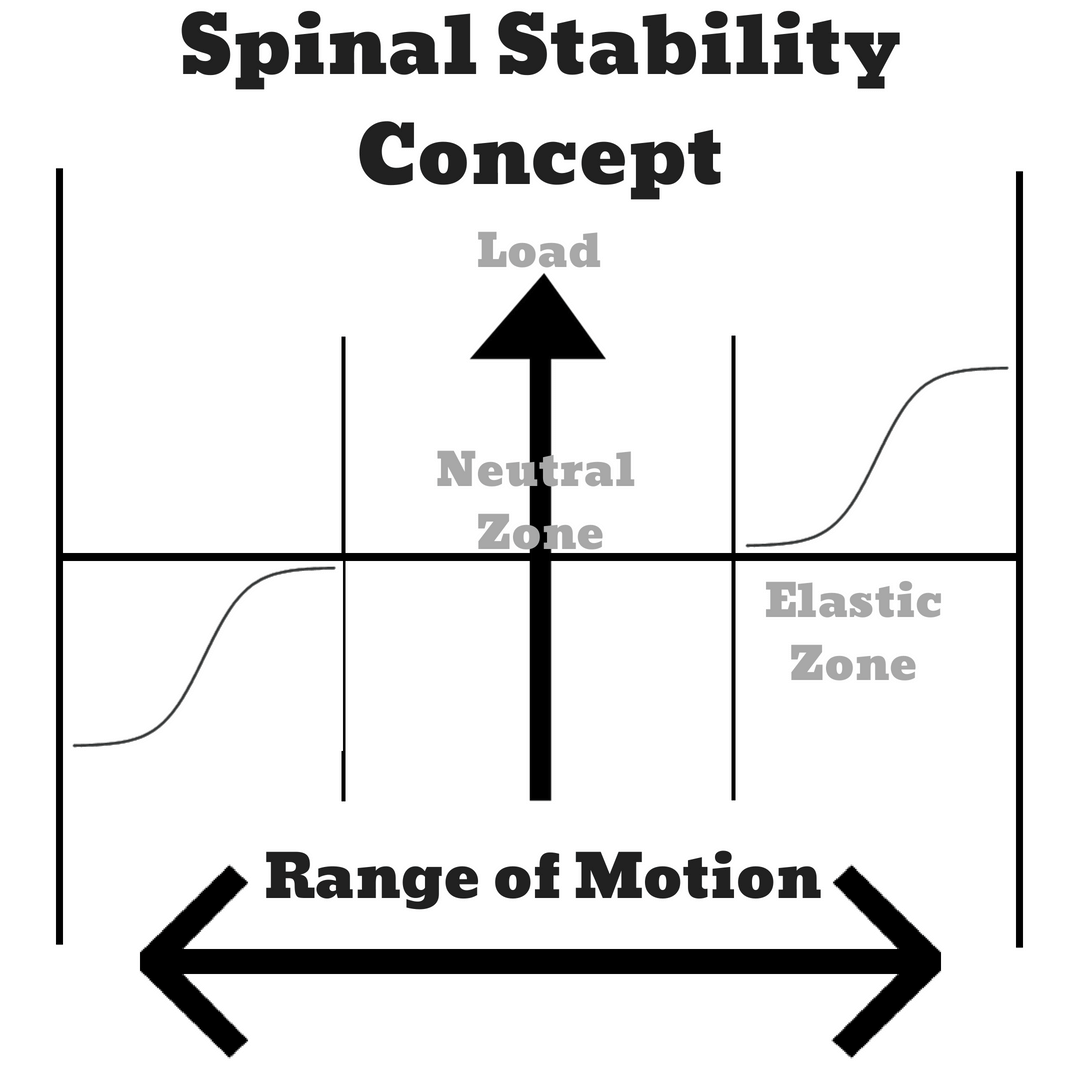
In sifting through the evidence for the origin of this term, we find terminology from Panjabi – neutral position and neutral zone. Panjabi created these terms based on experiments looking at how much force was required to change the intervertebral motion of segments (load-displacement measures). The zone was remnants of this specific measurement based upon the area that fell under a certain internal resistance, and the neutral position was the center point of the zone.
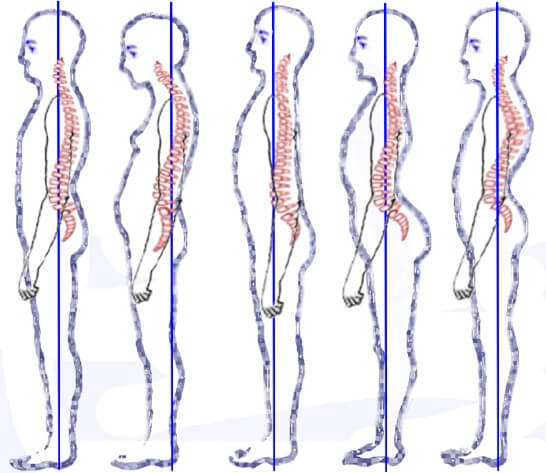
While this definition is very specific, it does not serve as a clinically applicable term, nor does it fit the format in which the terms are commonly used in a clinical setting. In contrast, what most individuals view to be a neutral spine is this midpoint between maximum lumbar flexion and maximum extension where the lumbar spine has a small arch (lordosis). This is the terminology that is most commonly applied to what we deem as the neutral spine.
Conversely, instead of it being a singular position, it should more likely be thought of as a zone – similar to the Panjabi reference. Generally, when individuals discuss the neutral spine position as described above, it is in reference to an erect standing posture. However, during activity – such as lifting something off the floor, squatting, etc. – we see the spine deviate from a set position and undergo varying degrees of lumbar flexion and extension. Even when participants are cued to execute the movement with a neutral spine (and under careful observation by experts such as Dr. Stuart McGill), we still see lumbar flexion occur. Within a squat, there is 40° of flexion occurring, 26° of flexion during a kettlebell swing, and 25° of flexion during a good morning. This elucidates the point of neutral spine being more a range than a specific position. If during most “functional” movements we see the spine flex up to approximately 40°, then what exactly is the neutral zone?
Is Lumbar Flexion Dangerous? Is it More Dangerous Than Neutral?
Hazard vs Risk
An important concept to understand as we go forward is the difference between hazard and risk. A hazard will be anything that could possibly do harm. In contrast, a risk will be the actual potential that a hazard has to cause harm. In essence, something may be a hazard, but unless the right exposure is there, it cannot really create harm, thereby holding little risk.
Analogies can really help explain this concept. Let’s consider the risk of being bitten by a shark. Shark attacks are a hazard, but if you never enter water where sharks are, you are not exposed to them, leaving you with little risk of being exposed to a shark attack. Without exposure to the hazard, there is little-to-no risk. This blog does a fantastic job of breaking this down more if you’re interested.
Assuming lumbar flexion is a hazard of some kind (which we will explore more), we need to examine the relative amount of exposure required to create a significant risk.
We have a large body of evidence that would support an argument that lumbar flexion does pose a possible mechanism to injury (some form of hazard). This comes from varying perspectives of mechanisms associated with flexion – repetitive flexion, long duration stretch, low compression rate, high compression rate, etc.
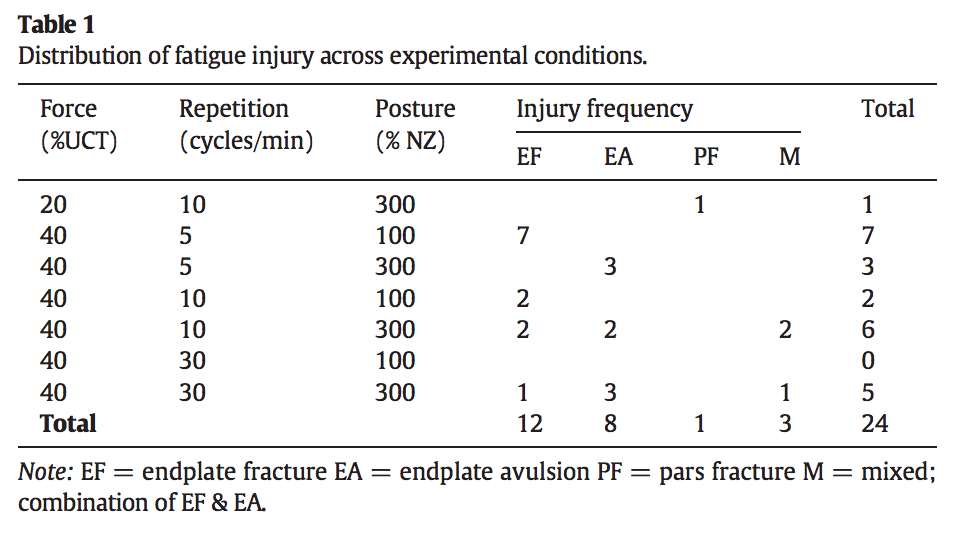
Most commonly, people associate lumbar flexion with disc injuries. However, we can also see from the work of researchers like McGill, Wade, Gooyers, and others that there is more than just discs that can be compromised with flexion-based activities. In particular, when we look at the work from Wade et al. 2014, we see that there was actually a higher incidence of endplate fractures than there was with disc failure with flexion. In regards to the disc, from these studies, we can see where the argument that the disc is most at risk with lumbar flexion and elevated rates of compression comes from.
If we take that information and run with it, we have what seems like a well-supported argument against activities utilizing a flexed spine – particularly with higher compression. This is the research that has supported the major trends in veering away from flexing the trunk, favoring the neutral spine instead. If we examine the majority of training programs for athletic development, physique enhancement, or rehabilitation, the overwhelming majority would likely consist of activities focusing on a neutral spine (planks, deadbugs, etc.).
However, we should not stop investigating the literature just yet. We need to consider the full spectrum of information and investigate other plausible mechanisms of injury.
First, we have a plethora of research that shows disc pathology is not inherently causative of pain or decreased function. As research builds in this area, we are seeing that it appears to be a part of the natural aging process for these anatomical variations to occur. Second, we have information that shows the same injuries can occur in a “neutral” spine. These injuries range from the tears within the end plate adjacent to the transition zone, tears at the inner annulus, tears at the mid annulus regions, micro-structural damage, disc herniation, and end plate fractures. This list of possible “injuries” looks identical to that of the injuries resulting in a flexed spine.
What Makes Flexion Have an Increased Risk?
When we look at the research, there seem to be factors that modify the inherent risk associated with lumbar flexion. It appears that flexion can pose a greater risk with situations that have higher compression rates or compression load. In Wade et al. 2014, the group compared four situations: neutral spine and low-rate compression, flexed spine and low-rate compression, neutral spine and high-rate compression, flexed spine and high-rate compression.
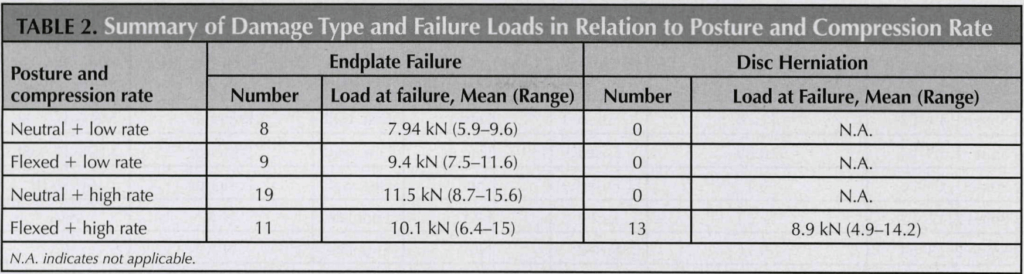
In both conditions of low-rate compression, the endplates fractured without the discs failing, and the magnitude of compression necessary to cause a fracture was not found to be statistically significant between neutral and flexion. In contrast, when compression rate increased, an interesting phenomenon was observed.
Similar to low-rate loading conditions, when high rates of compression were applied, there was not a statistically significant difference in compression load between spinal postures to induce an end plate fracture. However, while the neutral spine disc segments also all failed due to end plate fracture in both settings, the flexed spine showed diverging characteristics based on the loading rate. When high rate was introduced, 50% of the segments had wall failure and subsequent disc herniation. The load required for failure with disc herniation was lower than that of end-plate fracture. This demonstrates lumbar flexion when combined with high compression as having an elevated risk over neutral.
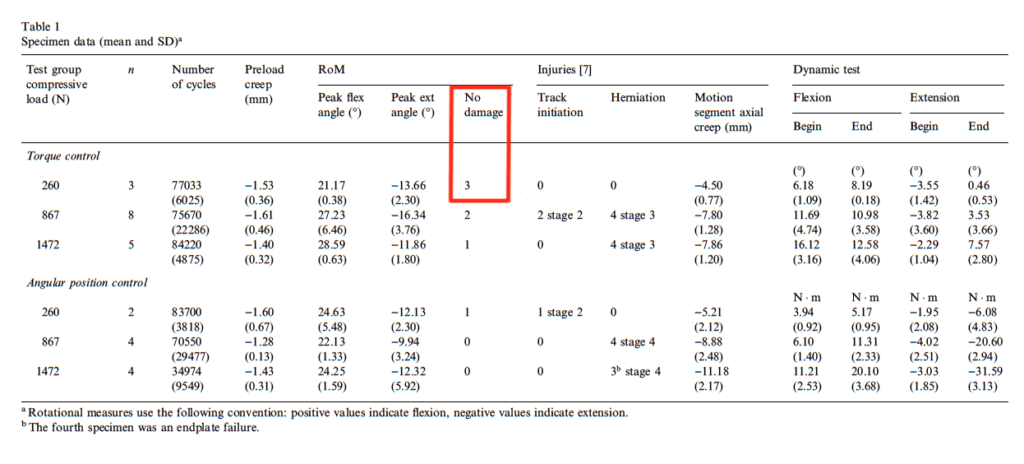
From Callaghan & McGill’s 2001 paper, we can see that herniations in the lumbar spine had a correlation with the applied load – not necessarily the number of motion cycles. In the study, they exposed specimens to three different loads (260, 867, or 1,472 N) for a maximum of 86,400 cycles through lumbar flexion and extension within a “neutral zone.” In the low-force group, none of the specimens had a herniation. In contrast, within the moderate- and high-load groups, there was a significantly greater number of herniations occurring – particularly with the high-load group.
Should We Fear Lumbar Flexion?
Looking at that prior paragraph, we could be led to arguing that flexion with load is dangerous, but is that the whole story? First, we should notice that within the Callaghan & McGill study, the range of flexion was within the neutral zone per the Panjabi formula. In addition, the work of Gooyers et al 2015 and Veres et al. 2010 show us we can see discs being challenged within the neutral zone.
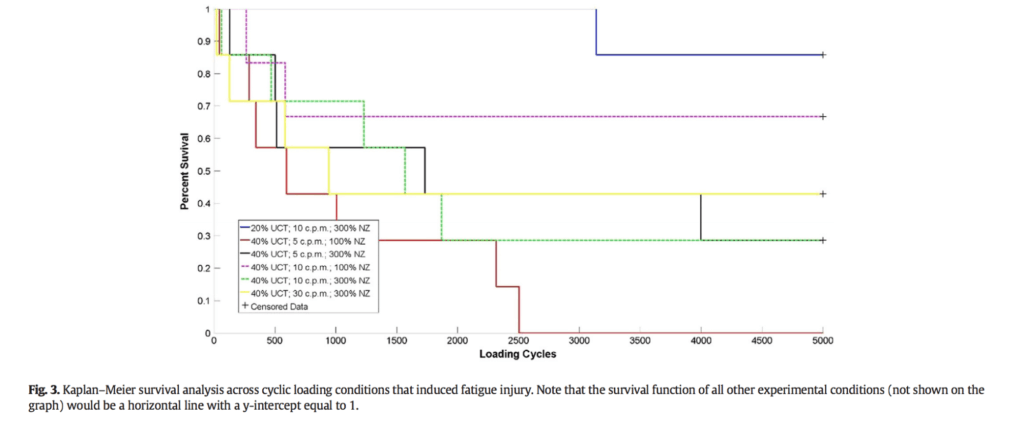
Gooyers et al. set up an experiment to compare three levels of compressive force (10, 20, and 40% of compressive tolerance) and three cycle rates (5, 10, and 30 cycles per minute) within two ranges – either the neutral zone, or 300% of the neutral zone – to a maximum of 5000 cycles. The authors stated, “the 100% neutral zone postural condition was intended to represent a lifting technique with sound mechanics (i.e. minimal lumbar spine motion), whereas the 300% condition was designed to bring isolated joints to end of natural physiological range.” Of the specimens, 23 (20%) experienced some form of injury related to either end plate fracture, avulsion fracture, or fracture of pars interarticularis. Of these injured specimens, 14 came from the group that was exposed to 300% of the neutral zone, whereas 9 came from the regular neutral zone. What is interesting to note is that one of the primary injuries that arose was a fracture of the pars interarticularis of the superior vertebrae (spondylolysis), which is most associated with hyperextension – not flexion. If we were to take out the pars fracture specimens from the results to look at injuries less associated with extension, we see the results change to 9 for the neutral range and 12 for the 300% neutral zone.
Veres et al. 2010 compared vertebral disc failure and vertebral end plate failure between a neutral and flexed vertebral spine position with pressure impulse stress. In essence, the vertebra were set to be either in a neutral zone or in 7° of physiological flexion (one segment). Then, the disc was pressurized to a specific level (8MPa), allowed 12-14 seconds to settle and be observed for failure, and then more pressure was added progressively. This format was repeated until all segments failed either via disc failure or end plate fracture. In most studies examining flexion versus neutral, the stress is repeated motion to failure; in this study, though, it was comparing high rate internal pressure. This paper helps to add depth to our understanding, as this mechanism is similar to what would be experienced in many sporting activities where an individual is compressed quickly – such as tripping and landing on their butt, or placing a heavy barbell on their back.
Their results demonstrated that the neutral spine is not safe from injury; in fact, the neutral segments experienced a higher percentage of disc failure during both impulse and gradual pressurization.

When examining many of the above papers looking at flexion, we should keep in mind the methods of the studies. In most of the studies, there was a range of continuous cycles between 5000 and 86,400. While this is a necessary component of researching variables, we should consider that this is not directly applicable to real life. It is pretty rare to find someone busting out 5,000 continuous reps of an exercise. Instead, we will see individuals perform significantly fewer repetitions and allowing time to recover and adapt from that stress. This returns us to our previous discussion of hazard versus risk. If flexion does pose a hazard, the apparent exposure in order to induce much risk is appearing to be quite significant and is unlikely to arise. There is also evidence to support that discs do have a capacity to adaptively strengthen and heal over time. In all of these studies examining spinal flexion as a mechanism of injury, we are left with an unrealistic situation for the disc to be able to adapt.
Most of the studies above are conducted on animal spines. This leaves us to infer transfer (which is not always consistent) from animal models to humans. Because of this, many scientists have begun to examine human cadavers for a more accurate representation of our tissues. This is an excellent step in the right direction for research, but we must remember a major caveat: This is not living and responsive tissue.
Essentially, the majority of the research on creating a causal relation of flexion and spinal degeneration of any kind has been done on cadaveric tissue. This is part of the scientific process, and many points can be inferred from these spinal models; however, there are distinct things that limit our capabilities of inferring knowledge from these studies.
For example, Contreras & Schoenfeld made an excellent point: “cadaveric tissue does not have the capacity to remodel.” In contrast to our deceased comrades, we are able to adapt and improve. Further, in these specimens, there is minimal to no resorption of fluid in the disc during unloading, which is strikingly different from living humans. Noguchi et al conducted a study looking at the impact of compressive force with flexion and extension of the spine in porcine models. Over 2700 cycles, pressure decreased by 26.8% due to creep stretch, fluid loss, and disruption of the annular wall. Those first two factors are very important, as discs are considered to be more at risk when dehydrated.
Many of the studies that have examined disc herniation associated with flexion moment or movement have not evaluated fluid loss or creep factors that are associated with the methodology used. This is an incredibly important factor that has not been addressed, and the data ignoring it is extrapolated to the real world, which skews people’s beliefs on the topic.
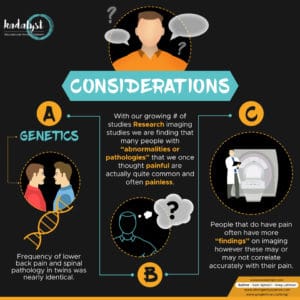
Considerations
Another aspect to discuss is the role of genetics. Many of us have seen that one guy who can bust out rounded-back deadlifts without any issue, and most people have also known someone who seems to injure their back every other week. Regardless of which side of the discussion you stand on, we can all respect that some individuals seem to be somewhat of an anomaly. While I’m very hesitant to say that the latter person couldn’t get better, we do have a significant amount of information showing there is a genetic link to these conditions.
Battie et al compared 45 pairs of twins with very different driving exposure – one doing a significant amount (5.4x average more driving) and one not. Although some would consider driving a risk for disc herniation due to the commonly flexed posture and whole body vibration exposure, the researchers did not find driving exposure to be associated with lumbar degeneration, disc signal intensity, or any other “abnormalities.” Specifically, disc degeneration did not differ between twins, except in the case of the lower lumbar spine where non-drivers actually had more frequent herniations than the drivers. Interestingly, it was more likely that if one twin reported lower back pain, the other would as well; the frequency of lower back pain between twin groups was nearly identical.
More studies have been emerged furthering this connection between pathoanatomical signs, pain, and relatedness. These reinforce a stronger correlation between genetics and pathoanatomical signs than other measures. In particular, we are seeing more information showing that many of these “abnormalities” are more an aspect of aging than an association of pain.
With our growing knowledge of base rates, much of what we had considered “damaged,” “injured,” or “pathological” is not necessarily accurate. However, this doesn’t mean we should disregard all findings.
Imaging should be primarily used to rule out sinister pathology such as cancer when there are signs pointing to it. Beyond those situations, imaging should generally not be utilized and can even potentially be harmful. As we have discussed, even if an individual has some form of “abnormality” on imaging, it does not mean it is associated with flexion or their current pain experience.
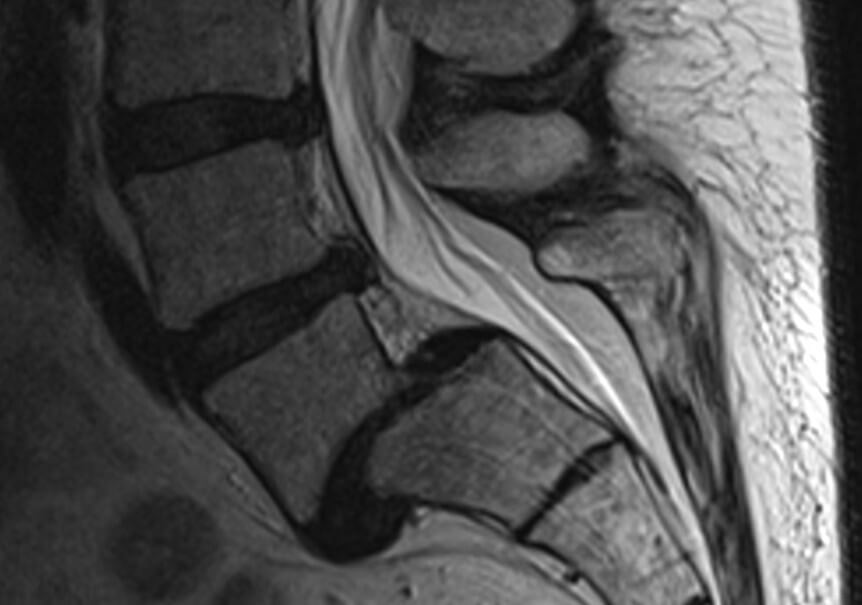
We do need to note that there are data to support that symptomatic individuals are more likely to have MRI findings than asymptomatic individuals. From the results, we can see that approximately 40% of individuals who are symptomatic will show some form of imaging finding, whereas approximately 20% of individuals who are asymptomatic will. This doesn’t mean that these findings are the cause of the pain and doesn’t dictate treatment.
Closing Thoughts
Unfortunately, the debate about lumbar flexion versus neutral is not simple and requires context, justifying the classic response of it depends. When discussing various sports, the recommendation will likely shift back and forth. From the flexed back of a cyclist to an extended back of a gymnast, sporting demands require inherently different postures and capacities. Pertaining to lifting, if we are looking at it from a perspective of low load or low rate activities such as picking up a pencil (and assuming the person does not have a high fear or belief that flexion is dangerous), it likely doesn’t matter whether they do so with a flexed or neutral spine.
As we get into lifting heavy objects or more grueling endeavors, “better” will likely shift more in favor of the neutral range. Currently, we have a number of papers that favor neutral while lifting; we do not have any favoring flexion.
If you find yourself working with the general population, a great strategy is to educate them on various options for lifting things: “stoop,” “semi-squat,” “golfers’ lift,” or the deadlift. Giving a variety of movement forms will allow the client to be prepared for more tasks, and building strength to be able to handle these positional changes is ideal.
If you are working with a barbell sport athlete, focusing on lifting volume with a neutral spine is going to be generally recommended. While the majority of training should have this emphasis, it may be necessary to have some training resemble their competitive positions (if this person deviates from neutral when lifting heavy). Training around improving lumbar flexion tolerance may be of benefit, but that is still unclear, and current evidence suggests focus should be placed on building strength in a neutral range.
Bonus: Is Lumbar Flexion Better Than Neutral?
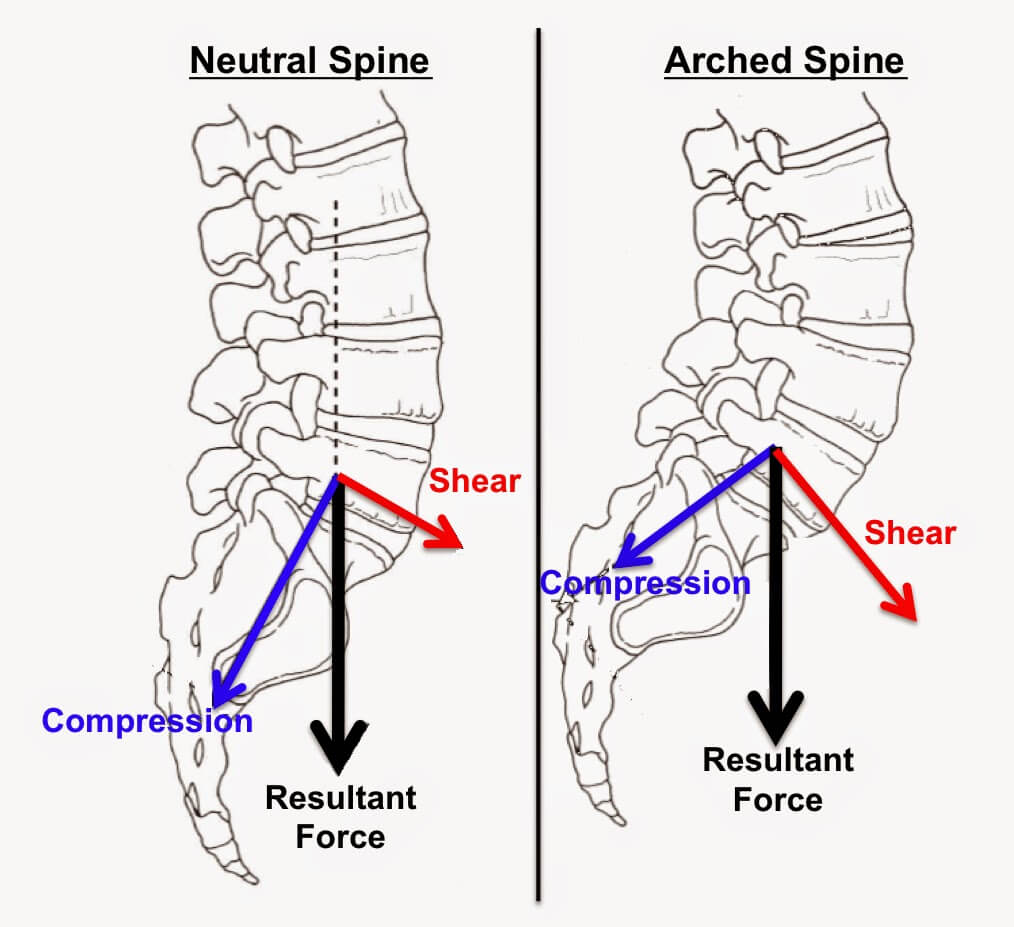
After reading the information presented above, most people would likely still side with the argument that neutral is better than flexion. We aren’t about to start saying that it’s best to always go with flexion; the evidence doesn’t show that. However, there are definitely situations in which flexion is both necessary and advantageous.
First, as we discussed prior, it is inevitable to not have some degree of flexion in certain activities. Good luck tying your shoes without flexing your back. Second, this depends upon what we are defining as “better.” From a standpoint of handling greater degrees of compression for cyclical load, flexion is not as tolerant as neutral. However, flexion is a required position for many activities and may pose a lower risk of disc failure with forces of impulse pressurization. For example, in sports such as wrestling and Brazilian jiujitsu (among others), flexion is a necessity, and there are many situations when flexing the spine is to the person’s advantage. Further, when we see many individuals performing maximal lifting events, it is not uncommon to see a change from neutral to flexion.
Beyond the need for it in activities of daily living and sports, lumbar flexion offers benefits to the spine that may not be achieved through a neutral position. Holm & Nachemson found that the intervertebral discs had increased aerobic metabolism in the outer parts of the annulus and nucleus pulposus following spinal movements. Lumbar discs rely on two main transport processes for nutrition: fluid flow and diffusion. Fluid flow is increased in flexed postures and helps to deliver nutrition better than a neutral position. In addition, a flexed posture reduces the stress at the apophyseal joints, which may be irritable from excessive extension activities. Does this indicate a better position? Not necessarily, but it may be in some instances. We know for sure, though, it is not something we need to fear.
Further Reading
- What I Learned About Injury Rates from Surveying 1,900 Powerlifters
- Squatting with Patellar Tendinopathy
- Training with Biceps Tendinopathy
Or, browse all prehab and rehab articles on the site.
References
- Setchell J, Costa N, Ferreira M, Makovey J, Nielsen M, Hodges PW. Individuals’ explanations for their persistent or recurrent low back pain: a cross-sectional survey. BMC Musculoskeletal Disorders. 2017;18:466
- Panjabi MM. The stabilizing system of the spine. part II. neutral zone and instability hypothesis. J Spinal Disord. 1992;5(4):390-396.
- O’Sullivan K, O’Dea P, Dankaerts W, O’Sullivan P, Clifford A, O’Sullivan L. Neutral lumbar spine sitting posture in pain-free subjects. Man Ther. 2010;15(6):557-561.
- Burnett A, O’Sullivan P, Ankarberg L, Gooding M, Nelis R, Offermann F, Persson J. Lower lumbar spine axial rotation is reduced in end-range sagittal postures when compared to a neutral spine posture. Man Ther. 2008;13(4):300-306.
- McGill SM, Marshall LW. Kettlebell swing, snatch, and bottoms-up carry: back and hip muscle activation, motion, and low back loads. J Strength Cond Res. 2012;26(1):16-27.
- Vigotsky AD, Harper EN, Ryan DR, Contreras B. Effects of load on good morning kinematics and EMG activity. PeerJ. 2015;6(3):e708.
- Potvin JR, McGill SM, Norman RW. Trunk muscle and lumbar ligalment contributions to dynamic lifts with varying degrees of trunk flexion. Spine. 1991;16(9):1099-1107.
- Kingma I, Faber GS, van Dieen JH. How to lift a box that is too large to fit between the knees. Ergonomic. 2010;53(10):1228-1238.
- Callaghan JP, Mcgill SM. Intervertebral disc herniation: studies on a porcine model exposed to highly repetitive flexion/extension motion with compressive force. Clin Biomech. 2001;16(1):28-37
- Wade KR, Robertson PA, Thambyah, Broom ND. How healthy discs herniate: a biomechanical and microstructural study investigating the combined effects of compression rate and flexion. Spine (Philla Pa 1976). 2014;39(13):1018-1028.
- Solomonow M. Neuromuscular manifestations of viscoelastic tissue degradation following high and low risk repetitive lumbar flexion. J Electromyogr Kinesiol. 2012;22(2):155-175.
- Gooyers CE, McMillan EM, Noguchi M, Quadrilatero J, Callaghan JP. Characterizing the combined effects of force, repetition and posture on injury pathways and micro-structural damage in isolated functional spinal units from sub-acute-failure magnitudes of cyclic compressive loading. Clin Biomech. 2015;30(9):953-959.
- Brinjikji W, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. ANJAR Am J Neuroradiol. 2015;36(4):811-816.
- Matsumoto M, Okada E, Toyama Y, Fujiwara H, Momoshima S, Takahata T. Tandem age-related lumbar and cervical intervertebral disc changes in asymptomatic subjects. Eur Spine J. 2013;22(4):708-713.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331(2):69-73.
- Veres SP, Robertson PA, Broom ND. ISSLS prize winner: how loading rate influences disc failure mechanics: a microstructural assessment of internal disruption. Spine (Philla Pa 1976). 2010;35(21):1897-1908.
- Porter RW, Adams MA, Hutton WC. Physical activity and the strength of the lumbar spine. Spine (Philla Pa 1976). 1989;14(2):201-203.
- Brickley-Parsons D, Glimcher MJ. Is the chemistry of collagen in intervertebral discs an expression of Wolff’s Law? A study of the human lumbar spine. Spine (Philla Pa 1976). 1984;9(2):148-163.
- Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of spontaneous resorption of lumbar disc herniation: a meta-analysis. Pain Physician. 2017;20(1):E45-E52.
- Contreras B, Schoenfeld B. To crunch or not to crunch: an evidence-based examination of spinal flexion exercises, their potential risks, and their applicability to program design. Strength & Conditioning Journal. 2011;33(4):8-18.
- Noguchi M, Gooyers CE, Karakolis T, Noguchi K, Callaghan JP. Is intervertebral disc pressure linked to herniation?: An in-vitro study using a porcine model. J Biomech. 2016;49(9):1824-1830.
- van der Veen AJ, Mullender M, Smit TH, Kinga I, van Dieen JH. Flow-related mechanics of the intervertebral disc: the validity of an in vitro model. Spine (Phila Pa 1976). 2005;30(18):E534-E539.
- Holm S, Nachemson A. Variations in the nutrition of the canine intervertebral disc induced by motion. Spine (Philla Pa 1976). 1983;8(8).866-874.
- Adams MA, Hutton WC. The effect of posture on the fluid content of lumbar intervertebral discs. Spine (Philla Pa 1976). 1983;8(6):665-671.
- Battie MC, Videman T, Gibbons LE, Mannien H, Gill K, Pope M, Kaprio J. Occupational driving and lumbar disc degeneration: a case-control study. Lancet. 2002;360(9343):1369-1374.
- Battie MC, Videman T, Kaprio J, Gibbons LE, Gill K, Manninen H, Saarela J, Peltonen L. The twin spine study: contributions to a changing view of disc degeneration. Spine J. 2009;9(1):47-59.
- Varlotta GP, Brown MD, Kelsey JL, Golden AL. Familal predisposition for herniation of a lumbar disc in patients who are less than twenty-one years old. J Bone Joint Surg Am. 1991;73(1):124-128.
- Battie MC, Videman T. Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am. 2006;88(Suppl 2):3-9.
- Weiler C, Schietzsch M, Kirchner T, Nerlich AG, Boos N, Wuertz K. Age-related changes in human cervical, thoracal, and lumbar intervertebral disc exhibit a strong intra-individual correlation. Eur Spine J. 2012;21(Suppl 6):S810-818.
- Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. JOSPT. 2011;41(11):838-846.
- Brinjikji W, Diehn FE, Jarvik JG, Carr CM, Kallmes DF, Murad MH, Luetmer PH. MRI findings of disc degeneration are more prevalent in adults with low back pain than in asymptomatic controls: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015;36(12):2394-2399.
- Neumann, D. A. (2010) Kinesiology of the Musculoskeletal System. St. Louis, MO: Mosby Elsevier
- Hutchinson MR. Low back pain in elite rhythmic gymnasts. Med Sci Sports Exerc. 1999;31(11):1686-1688.
- Standaert CJ, Herring SA. Spondylolysis: a critical review. BJSM. 2000;34(6):415-422.
- Lehman G. Revisitng the spinal flexion debate: prepare for doubt. 2016.