Note: This article was the MASS Research Review cover story for September 2023 and is the first installment of a new type of MASS article called “From the Mailbag.” The purpose is to address questions from MASS readers (or questions that are frequently asked within the evidence-based fitness community). If you want more content like this, subscribe to MASS.
How much dietary fat do we really need? This is one of the most common questions that stumps even the most seasoned and experienced fitness pros from time to time.
Before one begins to answer this question, it’s really important to frame the question deliberately. When asking how much dietary fat we need, we must operationally define what “need” means. Are we trying to identify the minimum fat intake that prevents death? The minimum fat intake that prevents clinically relevant adverse effects? The minimum fat intake that is practically feasible? The minimum fat intake to support feeling good? The minimum fat intake that is compatible with optimal physical function? The answer to each question will be a bit different. So, for this article, I want to focus on some of the key outcomes that establish informative boundaries for daily fat intake targets. I also want to make something very clear on the front end: this article exclusively pertains to healthy adults with no underlying medical conditions, and it does not constitute medical advice. For personalized nutrition guidance, it’s always advisable to consult with a qualified professional with appropriate credentials and training.
Gallstone prevention
The gallbladder is a small organ located in the upper-right quadrant of the abdomen. Its primary function is to store bile, which is produced by the liver. When we eat a fatty meal, the gallbladder releases bile to facilitate the digestion of fat. Gallstones are small, hard, pebble-like objects that form when bile hardens within the gallbladder. In many cases, gallstones do not cause any noticeable symptoms. However, if they block a bile duct, they can cause a painful buildup of bile, and may eventually necessitate surgical removal of the gallbladder.
It’s been known for decades that gallstone formation is one of the most common side effects reported in clinical weight loss trials in which considerable amounts of weight are lost very quickly (1). Rapid weight loss programs can sometimes cause the liver to release extra cholesterol into bile, which can increase the risk of gallstone formation. Beyond the risk associated with very rapid fat loss, extreme fat restriction seems to independently increase the risk of gallstone formation. It’s possible this is driven by a notable reduction in bile release when dietary fat is restricted, which leads to a bunch of bile sitting around for extended periods of time.
In clinical weight loss trials in participants with obesity, you might be shocked to see exactly how extreme some of the intervention diets are. It’s not particularly rare to see diets in the range of 500-800 kcal/day, with single-digit levels of daily fat intake. In a fitness industry where people are sometimes ridiculed for ever suggesting someone should eat fewer than 1200 kcal/day, these numbers might seem a bit jarring (especially for participants who often weigh over 200 pounds!). Unsurprisingly, these types of diets have been shown on many occasions to increase the risk of gallstone formation. Fortunately, it seems that this risk can be dramatically reduced by adding some fat to the weight loss diet, and the necessary amount of fat is shockingly low. Based on the best available evidence, an extremely modest fat intake of only 7-12 g/day appears to be enough to largely counteract the negative effect of extreme fat restriction on gallstone formation (1).
Essential fatty acid intake
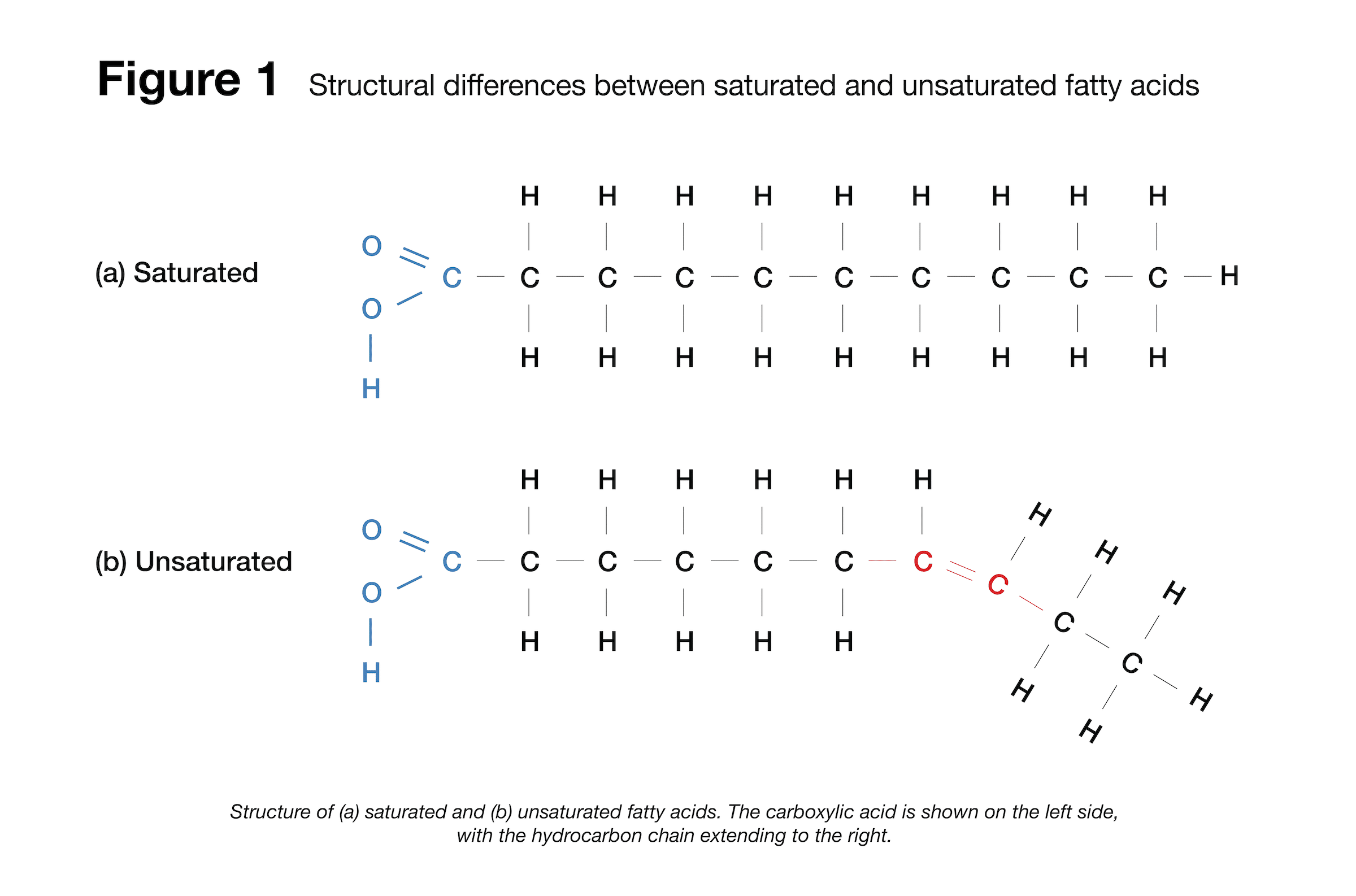
Another factor impacting dietary fat needs is our unavoidable need for essential fatty acids. Different fatty acids have different physiological roles in the body, and the structure of a fatty acid dictates its function. Fatty acids consist of a carboxylic acid attached to a hydrocarbon chain, and this hydrocarbon chain can vary in length. As a result, you’ll often hear about “short-chain,” “medium-chain,” and “long-chain” fatty acids. Another structural feature that can vary is the number of single and double bonds (Figure 1), which gives rise to the most recognizable distinction among fatty acids: saturated fats have all single bonds (with no double bonds), monounsaturated fats have one double bond (“mono” means “one”), and polyunsaturated fats have two or more double bonds (“poly” means “many” or “multiple”).
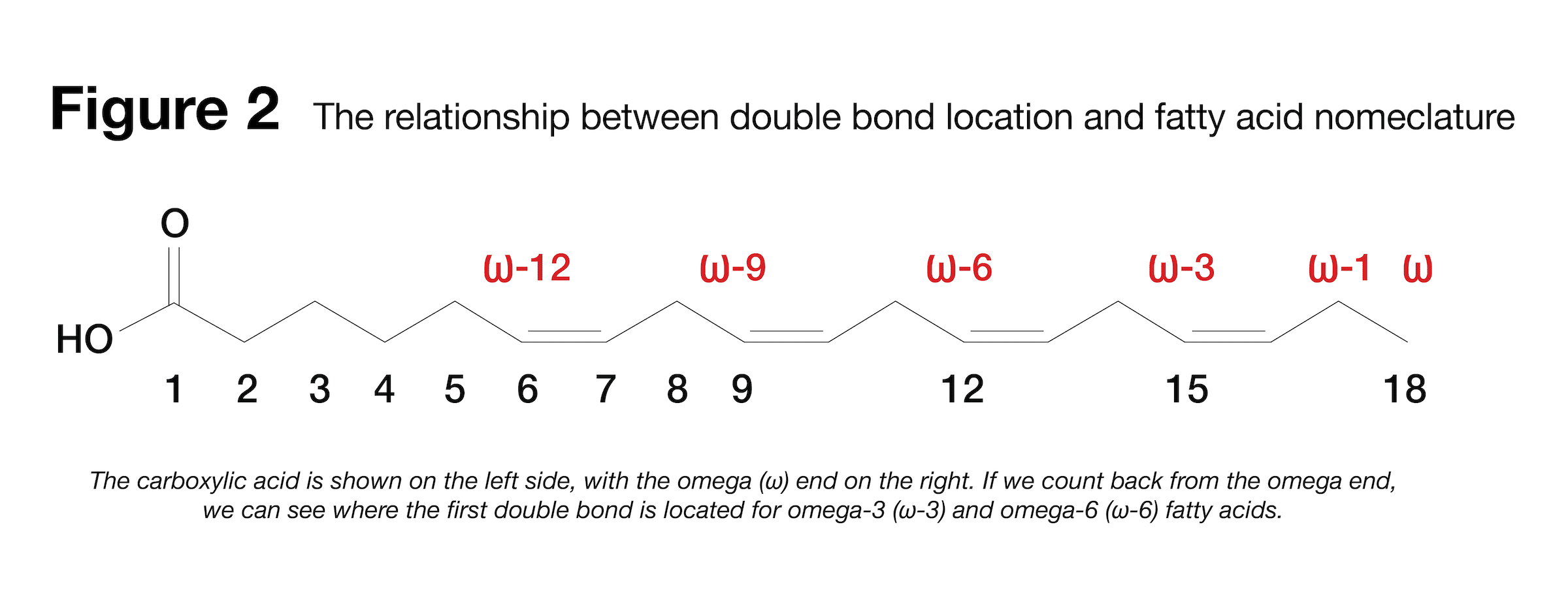
We can also distinguish fatty acids based on the specific location of their double bonds within the hydrocarbon chain – omega-3 fatty acids have their first double bond located at the 3rd position from the “omega” end of the chain, which is the end of the chain furthest from the carboxylic acid. Conversely, omega-6 fatty acids have their first double bond located at the 6th position from the omega end (Figure 2).
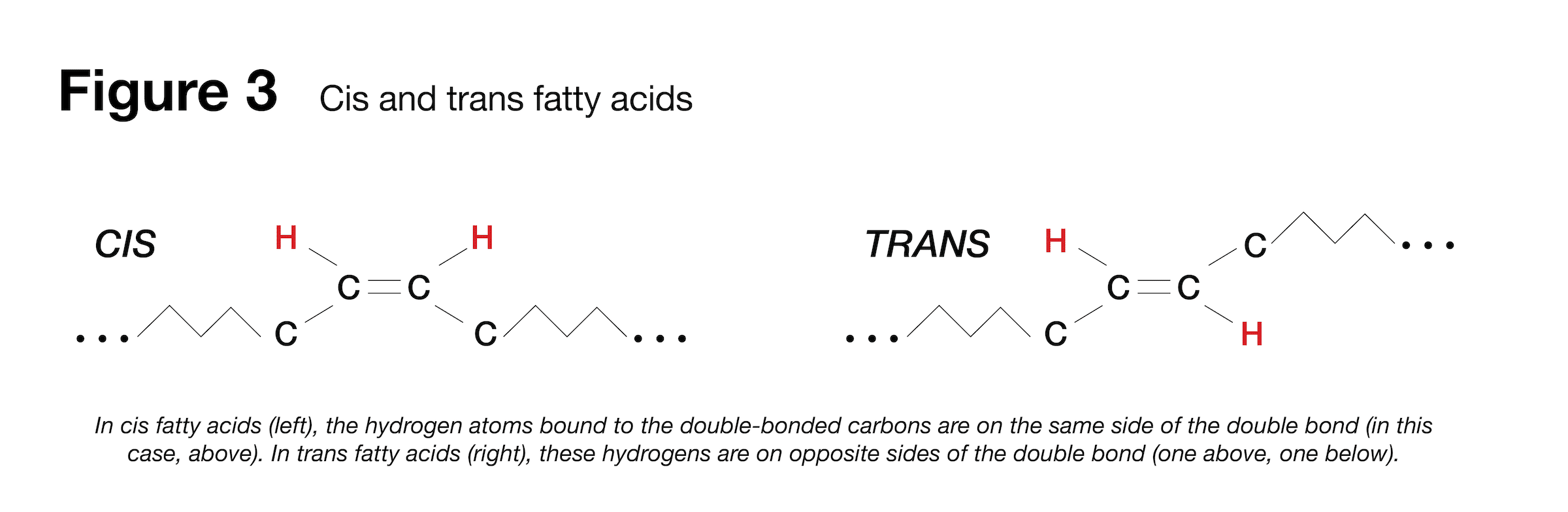
Finally, we can distinguish some unsaturated fatty acids from others based on the spatial orientation of their hydrocarbon chain. Unsaturated fatty acids have at least one double bond that joins two carbons together, with a hydrogen atom bonded to each carbon. If the hydrogen atoms are on the same side of the double bond, we’re looking at a cis formation; if the hydrogen atoms are on opposite sides of the double bond, we’re looking at a trans formation (Figure 3). This is where we get the terms “cis” and “trans” fatty acids from (which leads to the common recommendation to avoid trans fats).
Generally speaking, human beings are pretty good at rearranging the building blocks of fatty acids, rendering them largely interchangeable. We have all the enzymatic machinery necessary to chop up long fatty acid chains into shorter ones, build upon shorter ones to make longer ones, and swap between saturated and unsaturated bonds. However, there’s a major exception: omega-3 and omega-6 fatty acids. We lack the necessary enzymes to place a double bond at the 3rd and 6th position of these long-chain fatty acids, but sufficient omega-3 and omega-6 availability is considered essential for optimal health. As a result, we need to get omega-3 and omega-6 fatty acids from the diet. But exactly how much do we need?
Surprisingly, that question is hard to answer. While we know that omega-3 and omega-6 fatty acids are essential in nature, clinically relevant deficiencies of these fatty acids are so rare that it’s challenging to confidently identify minimum dietary targets to support health. As a result, some governing bodies have set “adequate intake” levels based on the median intake that happens to be observed among healthy individuals. Adequate intake levels of linoleic acid (the primary dietary source of omega-6) are 17 g/day for males and 12 g/day for females (2). However, some have argued that most adults should be able to get by with an intake of only 3-6 g/day of linoleic acid (3). Adequate intake levels of α-linolenic acid (the primary dietary source of omega-3) are 1.6 g/day for males and 1.1 g/day for females (2). If you’re wondering how the fatty acids in fish oil (EPA and DHA) fit into this equation, our bodies can use α-linolenic acid to produce EPA and DHA. If we look at a collection of recommendations from different countries, we tend to see intake targets around 1.4-2.5 g/day for total omega-3 fatty acids, with 140 to 600 mg/d coming from a combination of EPA and DHA (4).
When converting this to a daily target for total fat intake, we have to consider the concentration of omega-3 and omega-6 fatty acids within the actual foods and oils you consume. For example, you might say that safflower oil and peanut oil are both sources of linoleic acid (omega-6), but safflower oil is over 70% linoleic acid by weight, whereas peanut oil is around 20% linoleic acid by weight. Similarly, you could say that chia seeds and walnuts are both sources of α-linolenic acid (omega-3), but the oil from hemp seems is over 60% α-linolenic acid by weight, whereas the oil from walnuts is around 10% α-linolenic acid by weight. All in all, this creates a murky picture when trying to set minimum fat targets: there’s a lack of clarity about the actual daily requirement for these specific fatty acids, and dietary sources vary considerably in terms of their essential fatty acid concentration. However, if you’re looking for a rough heuristic to summarize this information, it seems reasonable to suggest that someone could meet their needs for essential fatty acid intake by consuming at least 20-30 g/day of fat, especially if they’re supplementing with essential fatty acids or intentionally selecting highly concentrated food sources.
Fat-soluble vitamin absorption
If you thought this section would bring a precise target with more clarity than the previous section, brace for disappointment. In lieu of a massive literature review, I’ll save you some time and provide a simple summary: vitamin absorption is complicated. We see all sorts of interactions among micronutrients, such that some are absorbed less in the presence of certain micronutrients, but absorbed more in the presence of others. Based on a combination of biochemistry and intestinal physiology, we know that dietary fat should facilitate the absorption of fat-soluble vitamins (which are vitamins A, D, E, and K). However, when it comes to the research exploring exactly how much it matters and exactly how much dietary fat is needed (and when it should be ingested), the findings are all over the place.
For example, one study found that short-term vitamin D absorption was improved by a low-fat meal (11g) rather than no meal or a high-fat meal (35g), but it didn’t make a big impact on long-term vitamin D levels (5). Some studies have indicated that the fat content of a meal meaningfully impacts vitamin E absorption (6), while other studies find no substantial impact (7). It gets even messier when branching out from single-meal absorption to longer time scales (several months) when assessing dietary fat intake and adequacy of fat-soluble vitamins, because fat-soluble vitamins can be stored in body fat and other tissues for later use. As a result, a person’s circulating levels of a fat-soluble vitamin aren’t necessarily reflective of their recent dietary habits. We know that medical conditions involving fat malabsorption considerably increase the risk of fat-soluble vitamin deficiencies (8), so we know (by extension) that a zero-fat diet would not be suitable for enabling adequate absorption. However, when it comes to supporting fat-soluble vitamin absorption, a clear and concise daily minimum fat target eludes us.
The most common recommendation is to aim for at least 10% of calories coming from dietary fat in order to support fat-soluble vitamin absorption (9). That amounts to 11 g/day for a 1,000-kcal diet, 22 g/day for a 2,000-kcal diet, and 33 g/day for a 3,000-kcal diet. This is a great example of why percentage-based dietary recommendations have some pretty big limitations – I don’t believe vitamin needs go down when you decide to cut your calories, but that’s an unspoken assumption of any percentage-based recommendation in this scenario. People who make percentage-based recommendations generally assume that you’re eating somewhere around 2,000 to 2,500 kcal/day, so we can probably reframe this 10% of total energy target as 22-28 g/day of fat intake, give or take. In the interest of using round numbers that are easier to remember, we can call this 20-30 g/day – after all, what’s the harm in rounding an inherently imprecise number?
Sex hormone levels
At this point, we’ve discussed the non-negotiable elements of minimum dietary fat targets: regardless of goal, we simply shouldn’t be okay with adopting a diet that meaningfully increases the risk of gallstone development, inadequate essential fatty acid intake, or inadequate fat-soluble vitamin absorption. These outcomes are (from my perspective) categorically unacceptable, which is why I’ve never (and probably will never) get on board with a diet recommendation involving less than 30g/day of fat. Having said that, we’re now venturing from non-negotiable necessities to an outcome that is absolutely desirable, but sometimes sacrificed in the pursuit of certain athletic endeavors. Many studies have shown that reductions in fat intake can lead to reductions in circulating sex hormone levels. Few lifters would consider that to be an ideal outcome, but we also know that decreased sex hormone levels are commonly observed in a variety of competitive endeavors, such as endurance sports and physique sports.
I’ve written about this topic previously in MASS, so I’ll only hit the highlights and summarize the literature in this article. Back in 2021, Whittaker and colleagues conducted a meta-analysis exploring the relationship between dietary fat intake and testosterone levels in men (10). They assessed short-term (2-10 weeks) interventions comparing low-fat diets (~19% of energy intake on average) to higher-fat comparator diets (~39% of energy intake on average) with similar total energy content in healthy, approximately weight-stable participants. They ended up including six studies with 206 total participants, and the analysis revealed that low-fat diets induced statistically significant reductions in total testosterone, free testosterone, dihydrotestosterone (DHT), and urinary testosterone, with non-significant reductions observed for luteinizing hormone and sex hormone binding globulin. Similar effects have been observed for estrogen levels in women; a meta-analysis from 1999 (11) reported that changing from a high-fat (29-46% of energy) to a low-fat (12-25% energy) diet reduced estrogen levels, with particularly large drops observed when fat was dropped below roughly 20% of total energy intake.
With these findings in mind, it seems very justifiable to suggest that studies support the recommendation to keep fat intake at or above 20% of energy to prevent drops in sex hormones. You could make a defensible argument that this should be 25% instead of 20%, but in the spirit of identifying absolute bare minimums, I’ll err toward the lower number. Having said that, there are a few important caveats to highlight. First, it would be inaccurate to say that more fat is always better, as excessive carb restriction has also been shown to reduce sex hormone levels. Second, it’s probably not ideal to frame fat intake as a percentage of total energy intake, as a super-low-calorie diet wouldn’t be expected to reduce the fat intake needed to support circulating sex hormone concentrations. If we assume a caloric intake of 2000-2500 kcal/day, the 20% of energy figure would lead us to a lower fat intake boundary of about 45-55 grams per day. To account for uncertainty, imprecision, and inter-individual differences, I personally would expand this range to around 40-60 grams per day. This range generally matches my observations as a coach and competitor, for what it’s worth.
Third, I want to be clear that low fat intake is not the only factor driving low sex hormone levels in endurance athletes and physique athletes. In many cases, the independent impact of dietary fat is dramatically smaller than the impact of insufficient energy intake (relative to training load and total daily energy expenditure), and insufficient energy stores (in the form of fat mass). In other words, it’d be incorrect to say that eating at least 40-60 grams of fat per day is enough to be confident that your sex hormone levels will stay within preferred ranges – if you’re absolutely shredded and/or dramatically underfueling, reductions in circulating sex hormone concentrations are often unavoidable. So, adequate fat intake levels appear to support typical sex hormone levels, but they certainly don’t guarantee typical sex hormone levels or attenuate drops driven by more impactful factors.
Practical considerations
Now that we’ve covered the physiological and biochemical stuff, I want to briefly mention some practical considerations that contribute to “realistic” lower boundaries for fat intake. First, the presence of dietary fat tends to make a diet more satisfying by influencing the taste, smell, mouthfeel, and hedonic properties of meals (12). Ask any coach who has ever tried to recommend an extremely low-fat diet – clients tend to report a high level of diet dissatisfaction very shortly after the switch, and adherence slips.
Even if we set hedonic preferences aside, it’s exceedingly impractical to shoot for extremely low fat intakes for extended periods of time. If you’ve ever tried to do an extremely low-fat approach for a short period of time, you already know this to be true. Fat will find its way into your diet, whether you’re looking for it or not. Fat is present in most of the foods that we typically think of as protein or carbohydrate sources, and even the foods that we typically consider “approximately” fat-free have trace amounts of fat. On a food-by-food basis, this fat content seems negligible, but over the course of an entire day, you’d be surprised by how quickly it adds up. If you don’t believe me, open up any diet software and try to put together a 2,000-Calorie diet with less than 20g of total fat – it’s probably harder than you expect!
All of that is to say, most of this article has discussed minimum daily fat requirements based on physiological needs. When we set our sights on the practical aspects of actually designing and following an extremely low-fat diet, we tend to find that practicality and feasibility keep most peoples’ daily fat intake higher than the physiological bare minimums. This is purely a speculative hunch, but I suspect that this is one explanation for the fact that the United States and European countries recommend that fat makes up 20-35% of total energy intake, whereas some global bodies and Asian countries set the lower boundary at 15%. There are several countries in Asia with cuisines that are more compatible with low fat intakes, such that population-level average fat intakes are lower and lower fat intake recommendations are comparatively more feasible.
Conclusions
In the introduction, I mentioned that the topic of minimum dietary fat requirements can stump even the most seasoned and experienced fitness pros. While that might have seemed like a jab at fitness pros who are unable to confidently produce an answer to the question, it’s more like a compliment in many circumstances. If someone feels uncertain about the lower boundary of dietary fat requirements, it likely reveals that they have an appreciation for the complexities of the topic, and they are aware that the scientific evidence makes it exceedingly challenging to provide a singular, one-size-fits-all number with high confidence.
With this in mind, I think the discussion about theoretical minimum fat targets is addressed most effectively by going outcome-by-outcome to piece together a comprehensive understanding. If your goal is to merely avoid immediate medical events in the context of rapid fat loss diets lasting only a few months in duration, the daily minimum fat intake is actually quite low. So far, studies suggest that somewhere around 7-12 g/day of total fat intake should be enough to meaningfully attenuate the risk of gallstone formation that is commonly observed with very extreme low-fat weight loss diets. However, that’s not the only factor to consider when setting the lower boundary. If you’re interested in ensuring adequate intake of essential fatty acids, your target for total fat will depend entirely on the specific fat sources you’re selecting, but 20-30 g/day might serve as a decent (but very approximate) heuristic. This range (20-30 g/day) would also be a suitable “bare minimum” target if you’re aiming to support fat-soluble vitamin absorption. If you wish to support sex hormone levels, you probably don’t want to go too far below 40-60 g/day.
For convenience, these rough heuristics are presented in Table 1.
| Table 1. Rough (approximate) heuristics for absolute minimum fat intakes | |
| Outcome of interest | Approximate minimum intake (g/day) |
| Attenuate gallstone formation | 7-12 |
| Support essential fatty acid intake | 20-30 |
| Support fat-soluble vitamin absorption | 20-30 |
| Support sex hormone levels | 40-60 |
| Caveats: These are approximate values based on surprisingly limited evidence. They are absolute minimums, not recommendations. Needs might be slightly lower for people who are considerably smaller than the population average, and slightly higher for people who are considerably larger than the population average. This table exclusively pertains to healthy adults, and does not constitute medical advice. | |
These rough estimates refer to absolute minimums, not recommendations – I am not declaring or implying that low-fat diets are inherently superior to other dietary approaches in all cases. People often ask how much fat we truly need as a “bare minimum,” and that’s precisely what this article seeks to address. Whether or not a low-fat (or very-low-fat) diet is optimal, advisable, enjoyable, or tolerable for a given individual in a specific set of circumstances is a different conversation altogether.
Get more articles like this
This article was the cover story for the September 2023 issue of MASS Research Review. If you’d like to read the full, 100-page September issue (and dive into the MASS archives), you can subscribe to MASS here.
Subscribers get a new edition of MASS each month. Each issue includes research review articles, video presentations, and audio summaries. PDF issues are usually around 120 pages long.
References
- Festi D, Colecchia A, Orsini M, Sangermano A, Sottili S, Simoni P, et al. Gallbladder motility and gallstone formation in obese patients following very low calorie diets. Use it (fat) to lose it (well). Int J Obes Relat Metab Disord. 1998 Jun;22(6):592–600.
- Field CJ, Robinson L. Dietary Fats. Adv Nutr. 2019 Jul;10(4):722–4.
- National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. Chapter 5: Lipids. In: Recommended Dietary Allowances: 10th Edition. Washington (DC): National Academies Press (US); 1989.
- Aranceta J, Pérez-Rodrigo C. Recommended dietary reference intakes, nutritional goals and dietary guidelines for fat and fatty acids: a systematic review. Br J Nutr. 2012 Jun;107(S2):S8–22.
- Dawson-Hughes B, Harris SS, Palermo NJ, Ceglia L, Rasmussen H. Meal conditions affect the absorption of supplemental vitamin D3 but not the plasma 25-hydroxyvitamin D response to supplementation. J Bone Miner Res. 2013 Aug;28(8):1778–83.
- Jeanes YM, Hall WL, Ellard S, Lee E, Lodge JK. The absorption of vitamin E is influenced by the amount of fat in a meal and the food matrix. Br J Nutr. 2004 Oct;92(4):575–9.
- Traber MG, Leonard SW, Ebenuwa I, Violet PC, Wang Y, Niyyati M, et al. Vitamin E absorption and kinetics in healthy women, as modulated by food and by fat, studied using 2 deuterium-labeled α-tocopherols in a 3-phase crossover design. Am J Clin Nutr. 2019 Nov 1;110(5):1148–67.
- Siener R, Machaka I, Alteheld B, Bitterlich N, Metzner C. Effect of Fat-Soluble Vitamins A, D, E and K on Vitamin Status and Metabolic Profile in Patients with Fat Malabsorption with and without Urolithiasis. Nutrients. 2020 Oct 12;12(10):3110.
- Jéquier E. Response to and range of acceptable fat intake in adults. Eur J Clin Nutr. 1999 Apr;53(1):s84–93.
- Whittaker J, Wu K. Low-fat diets and testosterone in men: Systematic review and meta-analysis of intervention studies. J Steroid Biochem Mol Biol. 2021 Jun;210:105878.
- Wu AH, Pike MC, Stram DO. Meta-analysis: dietary fat intake, serum estrogen levels, and the risk of breast cancer. J Natl Cancer Inst. 1999 Mar 17;91(6):529-34.
- Drewnowski A, Almiron-Roig E. Chapter 11: Human Perceptions and Preferences for Fat-Rich Foods. In: Montmayeur JP, le Coutre J, editors. Fat Detection: Taste, Texture, and Post Ingestive Effects. Boca Raton (FL): CRC Press/Taylor & Francis; 2010.




