A recent meta-analysis sought to determine the relationship between daily step counts and all-cause mortality. The researchers started by scouring several databases to find all of the prospective cohort studies that quantified the relationship between step counts and all-cause mortality rate. From there, they extracted all of the relevant data, performed a pretty standard random-effects meta-analysis, tested for moderating variables, and assessed the certainty of their conclusions using the GRADE criteria.
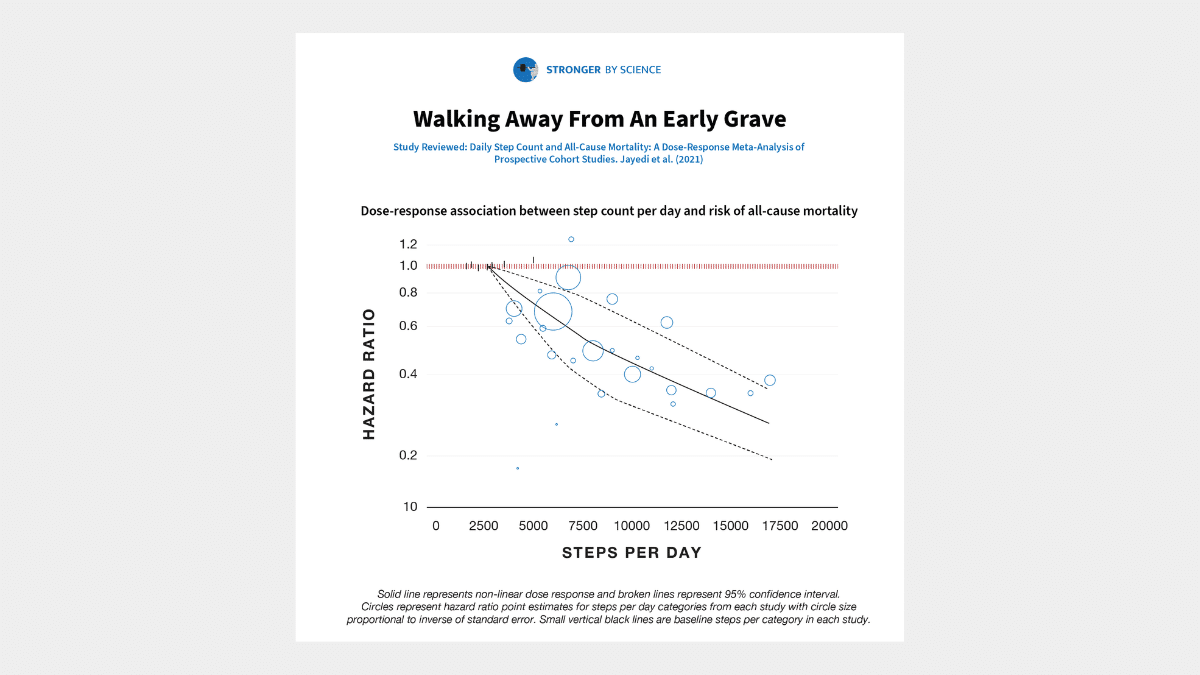
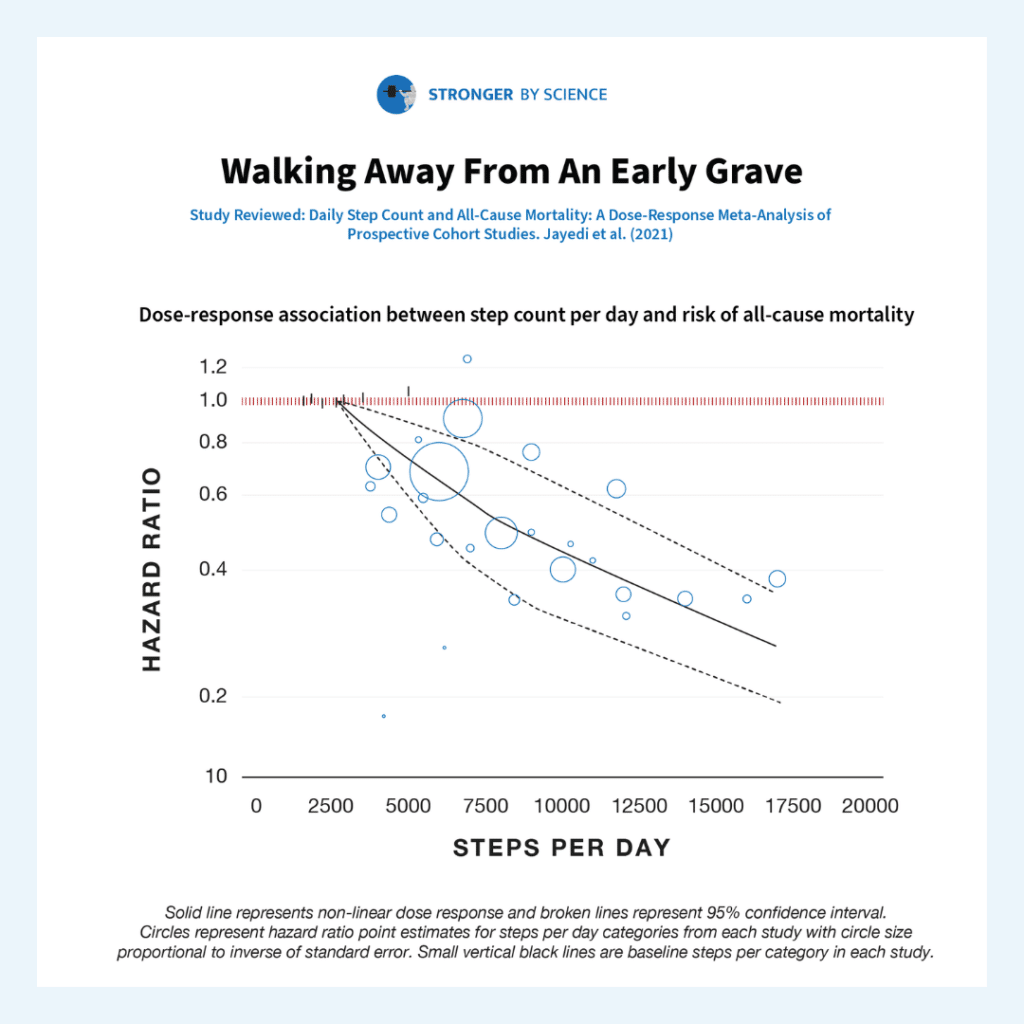
Seven studies were included in the meta-analysis, accounting for 28,141 total participants, 175,370 person-years, and 2,310 deaths. The researchers found that rates of all-cause mortality were about 12% lower per 1,000 steps per day (hazard ratio = 0.88; 95% CI = 0.83-0.93). The potential moderators examined (studies with longer versus shorter observation periods, studies from Europe versus the US versus Asia, studies with older versus younger participants, etc.) didn’t impact the findings to any meaningful degree – the hazard ratio fell within the range of 0.81-0.93 for all subgroups of studies tested. According to the GRADE criteria, we can have a high degree of certainty in the relationship between step counts and all-cause mortality. Comparing the lowest step counts to the highest step counts reported in the studies included in this meta-analysis, walking 16,000 steps per day was associated with a 66% reduction in all-cause mortality compared to walking just 2,700 steps per day. Stated conversely, walking 2,700 steps per day was associated with a three-fold greater risk of all-cause mortality than walking 16,000 steps per day.
Before interpreting these results, I want to make one thing crystal clear: I’m not falling into the trap of assuming that correlation implies causation. It’s entirely possible that people who are healthier simply tend to walk more than people who are less healthy, and daily step counts are therefore merely a proxy for general health, and don’t have an inverse causal relationship with all-cause mortality. However, I don’t think that’s the case – at least not entirely. For example, a 2015 meta-analysis found that group-based walking interventions, all lasting one year or less, led to significant decreases in systolic blood pressure, diastolic blood pressure, resting heart rate, body fat percentage, body mass index, total cholesterol, and depression scores, while increasing VO2max, 6-minute walk distance, and score on the SF-36 physical functioning inventory. Most walking intervention studies don’t use particularly strenuous walking programs either – generally 20-30 minutes of walking per day, which works out to ~2,400-3,600 steps for most people. So, if a bit of walking can beneficially modify ten different risk factors for all-cause mortality in less than a year, I think we can make a pretty strong case that the inverse relationship between step counts and all-cause mortality is more than mere association.
I think it’s worth contextualizing how striking these findings are. I’m sure most readers would agree that cigarette smoking isn’t great for longevity. However, smoking seems to be associated with ~70-80% higher rates of all-cause mortality. Relative to people who walk 16,000 steps per day, walking just 2,700 steps per day is associated with ~200% higher rates of all-cause mortality. It’s also not uncommon for people in the fitness industry to discuss the risks associated with obesity, and for good reason. Higher BMIs are associated with greater all-cause mortality risk. However, a BMI of 30 is associated with a ~4% greater all-cause mortality risk than a BMI of 23, and a BMI of 40 is associated with a ~74% greater all-cause mortality risk (Table D, “All participants, all studies”). Thus, you could argue that being very sedentary (relative to being very active, as the standard of comparison) is a larger independent risk factor for all-cause mortality than smoking status or obesity.
I think it’s easy for lifters to fall into the trap of assuming that being in the gym for a few hours per week and maintaining a healthy body composition are sufficient to maximize longevity, despite being relatively sedentary outside of the gym. Dedicated training is great, and building and maintaining muscle mass and strength will probably help you live longer (and maintain your ability to comfortably perform activities of daily living further into your twilight years), but there’s no substitute for simply moving more. Research suggests that adults in the US average ~5,100-6,500 steps per day. The present meta-analysis suggests that getting just 6,000 steps per day is associated with an all-cause mortality risk ~126% higher than the all-cause mortality risk associated with taking 16,000 steps per day. I’m sure that 6,000 steps plus dedicated resistance training is better than 6,000 steps with no resistance training, but it’s difficult to overstate the importance of simply being on your feet and moving a lot.
Before I wrap up, I want to make it clear that I’m not arguing that we should start sedentary-shaming people. If you have an office job, you don’t live in a walkable city, and you have a lot of obligations outside of work, it may be hard to carve out the time to get a lot of steps in. If you live in an unsafe neighborhood, it may be harder to get a lot of steps in. There are plenty of diseases that make it harder (or impossible) to get a lot of steps in. I just want you, as an individual, to be informed – if you want to live a long time, it never hurts to go for a walk.