We’ve analyzed both sleep and vitamin D research in MASS Research Review on several occasions. Throughout those articles, we’ve largely concluded that sufficient sleep is good, insufficient sleep is bad, and vitamin D supplementation has the potential to positively affect outcomes related to strength and hypertrophy (when baseline vitamin D levels are low), although the vitamin D literature is a bit inconsistent. However, we’ve never had an occasion to cover the intersection between vitamin D and sleep and discuss how the two might be interrelated. The presently reviewed study gives us such an opportunity, as it was a meta-analysis that sought to quantify the effects of vitamin D supplementation on sleep outcomes.
Before I get into the methods and results, I want to highlight the fact that this research question is not arbitrary – observational research seems to be hinting at the idea that insufficient vitamin D levels could negatively impact sleep. For example, a meta-analysis by Gao and colleagues pooled observational data from 9397 participants and found that vitamin D deficiency was associated with a higher risk of sleep disorders, poor sleep quality, short sleep duration, and sleepiness. Similarly, a meta-analysis of observational data by Yan and colleagues found that subjects with sleep disorders had significantly lower serum vitamin D levels than healthy controls.
These findings might seem very compelling, but reverse causation is always a pertinent issue with observational vitamin D research. Our bodies synthesize vitamin D in response to sunlight exposure, and regions of the brain that control sleep have a high density of vitamin D receptors. So, it’s easy to imagine a straightforward scenario by which vitamin D, either from sunlight or dietary intake, plays a direct and causative role in regulating sleep. However, we can just as easily imagine a very different scenario, by which a person with severely impaired sleep is more likely to wake up later, take naps during the day, or pursue fewer outdoor activities (and other activities outside of the home) due to sleepiness. In such a scenario, poor sleep would reduce opportunities for morning and afternoon light exposure, which would lead to reduced vitamin D levels.
Fortunately, the presently reviewed meta-analysis restricted its scope to intervention studies, which alleviates some of these reverse-causation concerns. The researchers searched a number of databases to identify vitamin D supplementation interventions that assessed outcomes related to sleep quantity or quality. They excluded studies whose participants had medical conditions (or used medications) that might impact vitamin D metabolism, as well as studies shorter than four weeks in duration. Their search yielded 19 studies that met inclusion criteria, which included 13 randomized controlled trials. Study durations ranged from 8 weeks to 5.3 years, daily dosages ranged from 1000 IU (international units) to 7143 IU, and risk of bias was generally pretty low among the included studies.
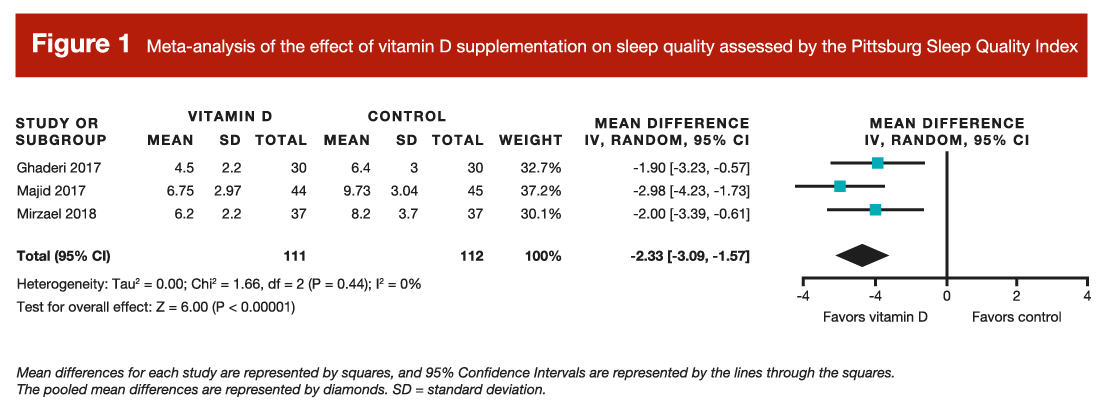
Unfortunately, the researchers were mostly unable to pool results together for quantitative analyses, largely due to a low number of studies and differences in study design, outcomes measured, and data reporting. A pooled quantitative analysis was possible for sleep quality, as measured by the Pittsburgh Sleep Quality Index, which quantifies sleep quality on a scale ranging from 0 to 21 (with lower numbers representing higher quality sleep). Results indicated that vitamin D supplementation was associated with a statistically significant improvement in sleep quality, which resulted in a score change of approximately 2.3 units (Figure 1). However, given the very small number of studies, this finding should be interpreted very cautiously. A few other outcomes were assessed by qualitatively summarizing the available literature. Generally speaking, the researchers found mixed results for disturbed sleeping, sleepiness, and symptoms of restless leg syndrome.
In summary, the available research provides mechanistic explanations for why vitamin D should impact sleep, observational examples where vitamin D appears to impact sleep, and interventions reporting weak and inconsistent results suggesting that vitamin D supplementation might have a favorable impact on sleep quality. I wish we had more clear and consistent evidence from interventions studies that would allow for a less ambiguous conclusion, but this is par for the course when it comes to vitamin D research. For example, Pilz and colleagues recently published a critical appraisal of recent randomized controlled trials on vitamin D, which outlined some study design considerations that likely reduced the likelihood of observing statistically significant effects on primary study outcomes. Similarly, Kiebzak and colleagues recently went into even greater depth about methodological considerations, which are probably promoting inconsistent findings among vitamin D studies and providing substantial challenges for those aiming to draw conclusions from the existing literature. In short, they argue that interpretation of the existing vitamin D research is difficult due to variations in assay format, study cohorts, data reporting, cutoffs defining deficiency, and measurement of pertinent variables to assist interpretation (such as sun exposure or sunscreen utilization).
Getting to the bottom of all existing vitamin D research is a lot to take on for a research brief, so for now, I’ll reiterate my position related to the majority of vitamin D-related outcomes: 1) there are clear downsides of excessive vitamin D levels, and clear downsides of insufficient vitamin D levels, and 2) targeted vitamin D supplementation can be a suitable strategy for keeping blood vitamin D within an ideal range, which appears to be around 75-100 nmol/L, give or take. There is a middle ground between recommending universal vitamin D supplementation and declaring vitamin D supplements entirely useless, and that’s where I find myself. However, when we restrict the scope of our interpretation to the sleep literature, vitamin D supplementation seems like a watered down version of a more potent intervention that may be accessible to a decent percentage of readers (depending on their schedule, geographical latitude, and local weather conditions).
Our bodies run on an internal “clock” (known as a circadian clock), which has a pronounced impact on our physiology. Our circadian rhythm impacts when we sleep, when we wake up, and when certain hormones increase or decrease throughout the day. Things with the potential to “adjust the time” on our circadian clock, and therefore shift our circadian rhythm, are known as zeitgebers, a German term that means “time giver” or “synchronizer.” Light exposure is, without question, the most impactful zeitgeber influencing our circadian rhythm. When skin is exposed to light, it’s certainly possible that vitamin D plays some role in conveying the message of light exposure to our brain structures that regulate circadian rhythm and sleep/wake cycles. However, in people with no severe visual impairments, light seems to most directly impact the circadian clock by interacting with the retina of the eye. I’m not an expert in eye physiology, neuroscience, or circadian biology, but my read of the literature is that retinal light exposure is far more impactful than any effect we might observe from shifting serum vitamin D levels. The retina conveys messages regarding light exposure directly to the brain centers involved with circadian rhythm entrainment, with no involvement of vitamin D in the process. We are, of course, talking about indirect retinal light exposure here – you should never stare directly at the sun.
While the data independently linking vitamin D supplementation to better sleep quality is spotty and inconsistent, you can make a much stronger case that morning light exposure is an effective intervention for shifting circadian phase and favorably impacting sleep quality and quantity. In fact, a review by Blume et al suggests that natural daylight exposure can promote earlier sleep times, increase sleep duration, and enhance sleep quality. They also noted that daytime exercise could potentially augment these favorable outcomes. The relationship between daylight exposure seems to be most pronounced when light exposure is of relatively higher intensity, occurs relatively earlier in the morning (but after sunrise, obviously), and persists for relatively longer durations of exposure. Nonetheless, light exposures as short as five minutes may be able to meaningfully impact circadian rhythms, effective morning light exposure can be intermittent (that is, it doesn’t have to be a long, continuous bout of exposure), even a cloudy day should provide enough light intensity to make a positive impact, and some morning (or early afternoon) light exposure is better than none. In fact, one study assessing the ability of light exposure to favorably shift circadian rhythms found that only 30 minutes of bright light exposure conferred 75% of the benefit observed with two hours of bright light exposure. Finally, it’s important to reiterate that the effects of light exposure are extremely time-specific; daytime light exposure is excellent for reinforcing proper circadian rhythmicity, but nighttime light exposure (especially to light in the blue wavelength spectrum) can disrupt sleep.
In summary, it’s possible that vitamin D levels play a small role in impacting sleep quality or quantity. However, if I was struggling with sleep, my first move would not be to reach for the vitamin D capsules. Rather, I’d aim for a comprehensive and multifaceted approach to sleep support, which would begin with adhering to some very basic sleep hygiene guidelines and avoiding excessive light exposure (and, in particular, blue light exposure) in close proximity to bed time. In addition, I’d make a focused effort to get some daylight exposure, especially in the morning and early afternoon. When possible, I’d try to incorporate some physical activity into that pursuit of light exposure, which could take the form of a leisurely walk, jog, or bike ride. If that combination of strategies was not promoting satisfactory sleep improvement, I might then consider some supplementation options (such as melatonin, glycine, or tart cherry juice), which have been discussed in a previous MASS article. In addition, if you notice that you’re consistently struggling to fall asleep due to worrying or anxiety (which may, ironically, include worrying about your inability to fall asleep), mindfulness training could be a promising option. Only after exhausting all of these strategies might I consider vitamin D supplementation as part of a sleep-promoting intervention, as the direct evidence (so far) isn’t particularly strong. Of course, if you are struggling with relatively severe sleep disturbances, the most straightforward approach would involve linking up with a medical professional early in the process to rule out certain medical conditions and conduct a formal sleep study (if necessary).
Note: This article was published in partnership with MASS Research Review. Full versions of Research Spotlight breakdowns are originally published in MASS Research Review. Subscribe to MASS to get a monthly publication with breakdowns of recent exercise and nutrition studies.