Some people favor very simple nutrition guidelines that eschew the smaller details: set a daily protein target, set a daily calorie target, get reasonably close to both on a consistent basis, and you’re good to go. In contrast, others promote an approach that dedicates considerable attention to secondary and tertiary nutritional variables, such as food source selection, meal timing, peri-workout nutrition, carbohydrate and fat ratios, and so on. I wanted to cover the presently reviewed study (1) in a research spotlight because I’ve seen smart, well-intentioned people citing it as evidence that it is worthwhile to allocate a considerable amount of attention and effort to minding some of the smaller nutritional details. I personally disagree with some of the popular interpretations that are floating around, but we’ll get to that soon – first, let’s discuss what the researchers did and found.
This was a crossover study, in which 9 free-living women with insulin resistance underwent two separate 14-day experimental conditions in randomized order (1). In one condition, they had a regular meal schedule consisting of six meals per day. In the other condition, they had an irregular meal schedule; it averaged six meals per day, but varied from three to nine meals on any particular day. Meals were provided during both experimental phases, and participants were instructed to maintain their typical physical activity habits. A 14-day washout period separated the two experimental conditions, during which participants reverted to their typical, self-selected eating habits.
The reported finding that seems to be garnering the most attention on the internet is that the thermic effect of feeding was significantly higher (by about 20.9kJ) after the regular meal pattern than after the irregular meal pattern (Figure 1). In addition, significantly larger GLP-1 responses to a standardized test drink were observed following the regular meal pattern in comparison to the irregular meal pattern. For additional context, GLP-1 is a peptide hormone associated with subjective appetite suppression and reduced energy intake, so higher GLP-1 levels are considered to be favorable with regards to satiety regulation. Given these two findings, a common interpretation of this study is that irregular meal patterns lead to a combination of lower total daily energy expenditure and attenuated GLP-1 responses to meals, which would intuitively be assumed to lead to greater hunger, more positive energy balance, and an increased likelihood of unintentional weight gain.
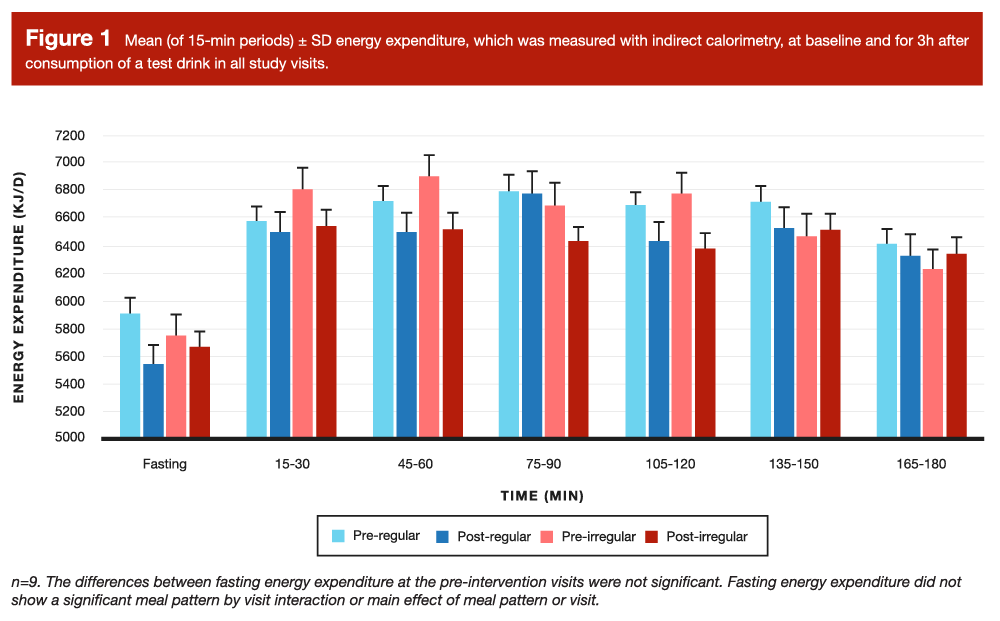
Personally, I don’t think these data are compatible with that interpretation. For starters, let’s take a closer look at the thermic effect of food data in Figure 1. If you focus on the post-regular and post-irregular bars, you’ll notice that they reflect very similar values in five of the six post-meal time points. Naturally, you might be wondering how these data reflect a significant difference between conditions. The answer is that the thermic effect of feeding is calculated as the post-meal elevation in energy expenditure, relative to the baseline (fasting) energy expenditure at that visit. It’s important to remember that this was a crossover design, so all participants served as their own control, and completed both study conditions. So, the “higher thermic effect of feeding” after the regular meal pattern was not purely influenced by greater absolute post-meal energy expenditure, but also by lower absolute pre-meal energy expenditure. In fact, if you look at the fasting energy expenditure value from before and after the regular meal pattern intervention, there was a fairly sizable drop (around 365kJ, or just shy of 90kcal).
Another important observation is that the baseline difference between conditions for the thermic effect of food was actually larger in magnitude than the post-test difference between conditions, despite the fact that participants served as their own controls in this crossover study, and they were consuming their habitual diets leading up to these baseline measurements. In other words, the study suggests that the two dietary patterns led to a ~20.9kJ difference in the thermic effect of feeding, but taking two different baseline measurements from the exact same participants led to differences even larger than that. It’s also worth noting that the thermic effect of feeding tends to last for more than 3 hours, so these measurements only represent the early phase of the effect. It’s entirely possible that a feeding intervention could simply shift the time course of the response in a manner that leads to a lower peak but more prolonged elevation; in such a scenario, a delayed response would be misinterpreted as an attenuated response when measured over only 3 hours.
If we take these energy expenditure values to be perfectly valid and reliable representations of the full thermic effect of feeding, it’s hard to get excited about the fact that the regular meal pattern led to a 20.9kJ (or ~5kcal) higher thermic effect of feeding value, while simultaneously leading to a 365kJ drop in resting energy expenditure. If we don’t take these energy expenditure values to be perfectly valid and reliable representations of the full thermic effect of feeding, then an alternative interpretation is that there’s a little bit of “noise” in the data (which is perfectly understandable) and an incomplete observation window, which also makes it hard to get too excited about a 20.9kJ increase. Either way, I think it’s really hard to claim that these differences in the thermic effect of feeding are going to have a physiologically meaningful impact on total daily energy expenditure, especially when the study does not provide comprehensive measurements of the other components of energy expenditure. They did estimate free-living energy expenditure using a wearable armband device (and found no significant difference between conditions), but, as discussed previously, these types of devices have measurement errors far larger than the actual treatment effect observed in this study (2).
In addition, as we’ve seen in multiple recent MASS Research Review articles, energy expenditure is complicated; changes in one component of total daily energy expenditure can impact a different component, and these interactions between energy expenditure components can differ based on an individual’s activity level, overall energy balance at the time of measurement, and other characteristics that vary from person to person (3). If we assume that the small difference in the thermic effect of feeding in this study is a true, reliable effect that would tangibly influence long-term body composition changes, we’d have to assume that a) this value was measured with exceptional validity and reliability, b) no other component of energy expenditure might undergo a compensatory change, and c) we wouldn’t experience any homeostatic nudge toward increased energy intake to offset the extra expenditure. This is a set of assumptions that I’m not inclined to make, so I’m doubtful that an increased thermic effect of this magnitude is worth chasing.
I’m even more skeptical of the practical relevance of the GLP-1 results. As I mentioned, the regular meal pattern appeared to be associated with a more pronounced GLP-1 response, which would generally be indicative of greater satiety. However, this study measured a variety of other satiety-related biomarkers, including adiponectin, leptin, PYY, and ghrelin; the researchers did not observe statistically significant effects for these outcomes, which means that only one of the five appetite-related biomarkers was significantly affected by the intervention. More importantly, this study assessed several different subjective appetite ratings (hunger, satiety, fullness, desire to eat, and prospective food consumption) at many time points throughout the study, in both fasted and fed states, and did not find a significant impact of the different meal patterns. The study also included an ad libitum test meal at the end of each meal pattern intervention, in which participants were encouraged to eat a pasta-based lunch until they felt “comfortably full.” Meal pattern did not significantly affect eating speed, eating duration, or total energy intake during this test meal. Given the non-significant effects of meal regularity on subjective appetite and ad libitum energy intake, the GLP-1 findings seem to lack practical significance.
Finally, I should also mention that the presently reviewed paper looked at a variety of outcomes related to general cardiometabolic health, including blood lipids, glucose levels, insulin sensitivity, and the glycemic response to a high-carbohydrate beverage. As these researchers discussed in their manuscript (1), some previous studies have identified statistically significant alterations in these cardiometabolic outcomes in short-term interventions with irregular meal frequency, but none of the measured cardiometabolic outcomes were significantly impacted in this study. More importantly, I personally question the clinical or practical relevance of the previous findings. The hypothesis driving this line of inquiry appears to involve some degree of concern that irregular, fluctuating meal frequency could cause some degree of metabolic derangement and drive unintentional weight gain (or, at minimum, hinder weight loss attempts). However, there’s already a whole body of literature evaluating several different variations of alternate-day fasting. In these studies, participants generally have at least two “fasting” days per week, in which they tend to consume ≤25% of their energy needs in a very brief feeding window (typically a single meal). In other words, the majority of alternate-day fasting studies involve an irregular meal pattern in which participants oscillate between 1 meal per day and 3-4 meals per day, and the effects on weight management and cardiometabolic outcomes tend to be neutral to positive (4). Of course, the alternate-day fasting literature differs from the intervention in the presently reviewed study, given that alternate-day fasting involves transient periods of reduced (but not increased) meal frequency relative to baseline, and generally induces a caloric deficit. As such, it’s theoretically possible that the purported metabolic perturbations associated with irregular meal frequency are only observed in the context of higher-than-normal meal frequencies or neutral to positive energy balance. Nonetheless, the alternate-day fasting literature casts doubt on the idea that irregular meal frequency per se is inherently unfavorable in all contexts, and (in my opinion) the studies investigating other types of irregular meal patterns don’t report metabolic perturbations that are large or consistent enough to warrant concern.
In summary, this study reports a significant impact of meal regularity on the thermic effect of feeding, which could be an artifact related to noisy measurements for baseline energy expenditure, and is probably too small to meaningfully impact total daily energy expenditure (even if we assume that all other components of total energy expenditure would remain reasonably constant). This study also reports a significant impact of meal regularity on GLP-1 responses, but none of the other satiety-related biomarkers were significantly affected, and neither were subjective appetite ratings or ad libitum energy intake. We’ve also got plenty of fairly long and well-controlled trials in which irregular meal patterns, in the form of various alternate-day fasting approaches, seem to have neutral or positive effects on weight management and cardiometabolic outcomes. These alternate-day fasting studies aren’t perfectly representative of the intervention assessed in the presently reviewed study, but they cast doubt on the idea that meal pattern irregularity is inherently unfavorable across all contexts. As such, I don’t think the typical dieter should be stressing out over an extra meal or a skipped meal here or there, as long as they’re generally on track with the big picture stuff (energy intake, total protein intake, and protein distribution).
If you really, really want to manage all the tiny details to fully optimize your meal schedule, even beyond the details of protein distribution and peri-workout nutrition, you could aim to incorporate some strategies that fall under the umbrella of chrononutrition. A deep dive is outside the scope of this article, but a fantastic article by Danny Lennon covers all you’d want to know about it, and provides strategies to help align your diet with some basic principles of circadian biology. Meal pattern regularity would be part of the approach, but there’s much more to it, such as establishing a consistent feeding window, aligning your feeding window with your sleep/wake (and by extension, dark/light) cycle, and shifting calories toward the early part of the day. These are evidence-based strategies with some degree of both mechanistic and applied research supporting them, but these are the types of strategies that generally offer a pretty low return-on-investment, and are only worth the hassle if you’re fully intent on optimizing every optimizable aspect of your diet.