If you walk into a commercial gym, strap on a head harness, and start performing a neck extension exercise, there is a decent chance that you will draw some looks and maybe some grins from the people around you. Direct neck training is uncommon for the general population, and it can easily look silly to someone who is unfamiliar with this type of exercise. However, unusual does not equate to ineffective, and no substitute exists for direct neck training if your objective is to grow and/or strengthen the neck musculature.
Neck Muscle Hypertrophy
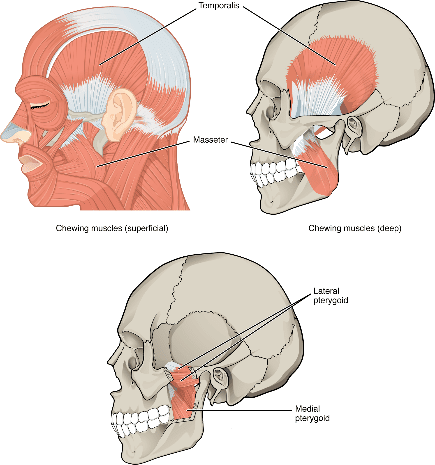
Many athletes perform strength training to enhance sport performance and decrease injury risk, but plenty of other people primarily care about lifting to be more jacked and/or become all around stronger human beings. With regard to physical appearance, no regions of the human body are more frequently visible than the face and neck. Except for the masticatory (i.e., chewing) muscles, whose strength and strength endurance have been reported to increase after a 6-week isometric jaw clenching exercise intervention, training the face musculature is not feasible (64).
However, you can develop a wide variety of neck muscles through direct neck exercises. Most people would not consider the tree trunk that connects Jeff King’s head to the rest of his body to be the pinnacle of aesthetics, but a proportionally thick neck can certainly contribute to a more powerful appearance that is evident in nearly all settings.
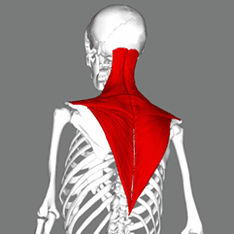
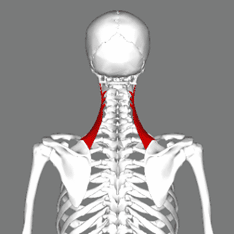
Some coaches and lifters have asserted that the neck muscles can hypertrophy from shrugs, rows, and deadlift variations, and that direct neck exercises are not necessary to achieve this increased muscle size. The trapezius and levator scapulae muscles constitute a sizable portion of the musculature on the back of the neck, with MRI measurements indicating that they comprise 34.6% and 8.3% of total neck muscle volume, respectively (38). Given that both muscles attach to the scapula, an exercise that does not load neck movement but does load scapular movement (e.g. shrugs) may have the potential to increase neck muscle size.
However, none of the other muscles that contribute to neck movement attach to the scapula, so they will be neglected if direct neck exercise is avoided. Thankfully, researchers conducted a study on this matter to investigate whether shrugs, rows, and deadlift variations are sufficient to increase neck muscle size. Conley et al assessed two groups of recreationally active subjects that performed four full body resistance training sessions per week for 12 weeks where each exercise was trained for 3-5 sets of 3-10 reps (17). The exercises included squats, push presses, bench presses, midthigh pulls (i.e., above the knee rack pulls), Romanian deadlifts, crunches, bent over rows, and shrugs. While one group exclusively performed this traditional resistance training protocol, the other group additionally performed a weighted neck extension exercise for 3 sets of 10 reps three times per week. Before and after the intervention, neck extension strength (i.e., max load for 3 sets of 10 reps) was tested, and MRI cross sectional area measurements were performed at nine neck muscle sites (reflecting 13 total muscles), including the trapezius and levator scapulae.
Following the intervention, the group that incorporated the neck extension exercise experienced significant increases in neck extension strength and neck muscle size at six of the nine sites measured, while no increase in neck strength or muscle size at any site occurred in the other group. Two of the muscle sites consisted of neck flexor muscles, so it is unsurprising that they did not exhibit any change for either group. However, the third site that exhibited no change in area for either group was the trapezius, which is a rather unexpected finding given the exercise selection. The authors did not discuss potential reasons for the apparent lack of trapezius hypertrophy, and speculating on this matter is beyond the focus of this article, but this intriguing outcome is worth highlighting nonetheless. The finding that levator scapulae hypertrophy was only observed in the neck extension group is also noteworthy, given that its anatomical attachments should enable it to function as a scapular elevator and allow it to be trained by shrugs.
Ultimately, my main takeaway from this study is that commonly performed back exercises (e.g. shrugs, rows, and rack pulls) may be insufficient to induce meaningful increases in neck muscle size and strength, but these adaptations can readily occur when direct neck exercise is included. Potentially, neck muscle hypertrophy may still occur in the absence of neck exercise after a more prolonged period of well-designed traditional training with appropriate nutrition that yields an appreciable increase in total body muscle. To my knowledge, however, the only other resistance training interventions that reported increases in neck muscle size to occur after training utilized direct neck exercise (14, 31, 65).
Neck Muscle Anatomy
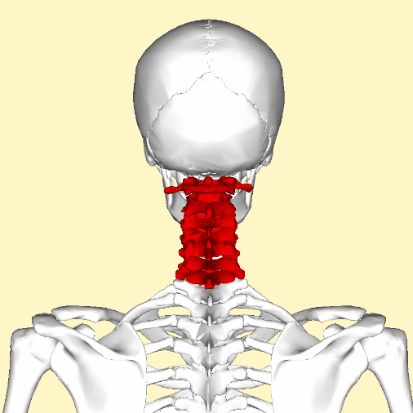
The cervical spine comprises the skeletal structure of the neck, and the joints formed among its seven vertebrae enable neck movement to occur in all three planes of motion (50).
Neck motion can occur as flexion (i.e., tucking the chin down), extension (i.e., looking up), side bending (i.e., tilting to the right or left), or rotation (i.e., twisting to the right or left).
Neck Flexion and Extension


Neck Side Bending


Neck Rotation


The upper and lower cervical regions can move independently from each other, so two opposite movements can simultaneously occur at different regions. As a result, retraction (i.e., pulling the head backward) can occur as the upper cervical flexes while the lower cervical extends, and protrusion (i.e., pushing the head forward) can occur as the upper cervical extends while the lower cervical flexes (49).
Neck Retraction and Protraction


The anatomy of the muscles that generate neck movement is quite complicated in part because they are often situated in different layers, which makes it difficult or impossible to visibly identify many of them.
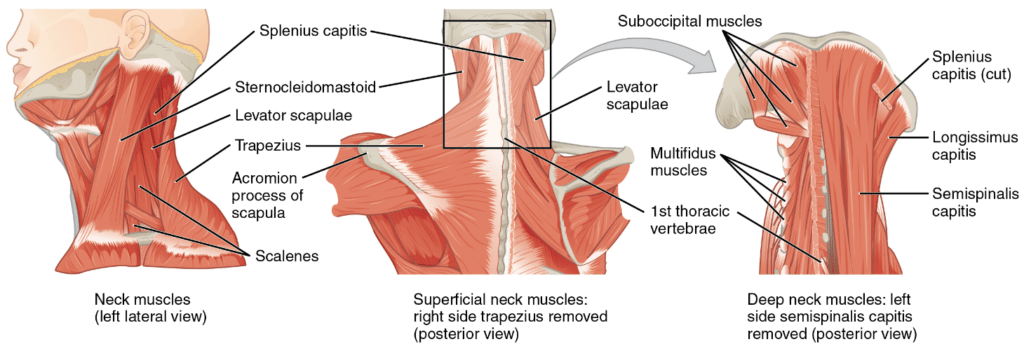
Additionally, a muscle that can generate a particular movement in one cervical region may not perform the same function in the other region. Most people will not be interested in exploring the nuance of these different muscles, nor is this required to incorporate effective neck training. Consequently, I summarized the data from several different studies on the neck musculature about which muscles will primarily be trained by each of the four neck movements. While most of the findings are congruent with one another, differences do exist, so some judgment is required with respect to functional classifications based on the body of evidence as a whole. For instance, the ability of the trapezius to contribute to neck movement is presently unclear. Biomechanical research reports this muscle’s upper region to have meaningful leverage to generate neck extension, side bending, and rotation torque (1, 47, 62, 67). However, EMG research has failed to detect any appreciable activation of the upper trapezius when exercises are performed for these three movements (25). Moreover, functional MRI research which measures changes in muscular fluid concentrations, a useful proxy for muscle engagement during an exercise which lacks some of the limitations of EMG research, has indicated that this muscle is not effectively trained with neck exercise (16). In light of the fact that all of the muscles suggested by this functional MRI study to function as neck extensors were reported to hypertrophy after the previously discussed neck extension exercise intervention, I can’t confidently assert that any neck exercise will meaningfully train the trapezius (16, 17).
Neck flexion is produced by the sternocleidomastoid, longus coli, longus capitis, and infrahyoid muscles (1, 12, 16, 47, 62, 67). Neck extension is produced by the levator scapulae, erector spinae, splenius muscles, semispinalis muscles, and suboccipital muscles (1, 16, 21, 47, 62, 67). Neck side bending is produced by the sternocleidomastoid, levator scapulae, erector spinae, and scalene muscles (1, 16, 47, 67). Neck rotation is produced by the sternocleidomastoid, splenius muscles, semispinalis muscles, and suboccipital muscles (1, 16, 67).
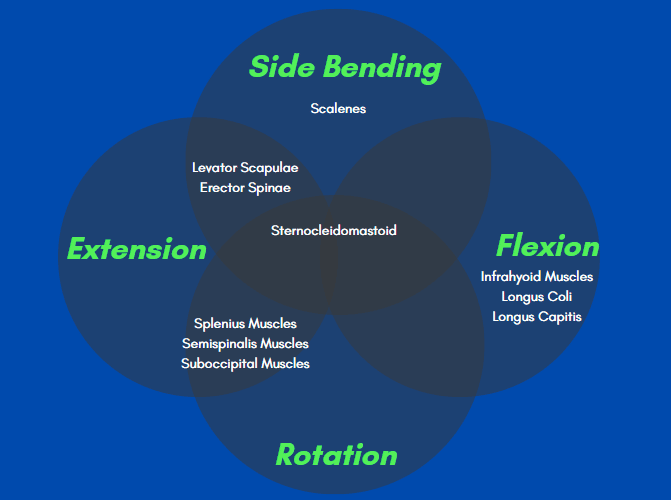
The main takeaway from this information is that you can target the vast majority of the neck musculature by using just two exercises because of the overlapping muscle functions. A combination of two movements, such as neck extension and neck flexion, will train nearly all of the muscles that would be targeted by performing one exercise for each of the four different movements. Consequently, supersetting a neck extension and neck flexion exercise together can be an efficient strategy to develop all regions of the neck in a brief period of time. If someone wishes to achieve every ounce of possible neck gains, a side bending neck exercise can also be included to ensure that none of the scalene muscles are neglected. However, if you are already utilizing extension and flexion exercises, I suspect that the overall effect of also including a side bending exercise would be minimal.
Neck Exercise
The exercises that you can utilize for direct neck training are quite simple. You can perform neck extension, flexion, or side bending exercise while lying atop a bench as you train the specific motion with a weight plate held against your head to provide resistance. For extension, you would lie on your stomach with the plate held on the back of your head. For flexion, you would lie on your back with the plate held on the front of your head. For side bending, you would lie on your side with the plate held on the side of your head. Each of the exercises will be most comfortable when wearing a beanie.
Neck Extension with Plate


Neck Flexion with Plate


Neck Side Bending with Plate


To ensure that the exercises are effectively targeting the muscles in the neck rather than those elsewhere in the body, make sure that you are merely using your arms to keep the weight in position rather than actively contributing to moving the weight. Nobody cares how much weight you neck curl, so keep your technique strict and leave your ego at the door. With regard to load selection, it is worth noting that neck flexion strength will be lower than extension strength (24, 47). If you have a head harness available, this fairly inexpensive tool can also be used to load neck extension exercise with an elastic band, cable machine, or free weights such as a kettlebell or weight plate.
Neck Extension with Harness


Given gravity’s vertical line of pull, free weights are not a viable modality to train neck rotation, but you can load this movement with a sheet band (e.g. TheraBand) wrapped around the head to apply tension when turning to either direction.
Neck Rotation with Band


Alternatively, you can manually apply external resistance to load any neck movement. This strategy can allow you to perform neck training and achieve a neck pump in nearly every environment, whether you are riding a bus, waiting for a job interview, or in between acts of your favorite play at the theater. If you opt to utilize manual resistance, you can readily individualize the level of resistance by adjusting how much pressure you apply through your hands to accommodate a particular rep range.
Neck Extension with Manual Resistance


Neck Flexion with Manual Resistance


Neck Side Bending with Manual Resistance


Programming Recommendations
If you are unaccustomed to neck training, you can likely progress with only a minimal time investment given the potency of a novel stimulus. A 10-week machine neck extension training intervention, consisting of a single set of 8-12 reps to volitional failure once per week with healthy untrained subjects, increased mean isometric neck extension torque by 6.3% to 14.3% depending upon which joint angle was tested (37). While a single set per week can be sufficient to enhance neck strength, including a second set has unsurprisingly been found to be even more effective. The lead researchers who directed the aforementioned study also conducted a similarly designed 12-week machine neck extension training intervention that included an additional group performing one set twice per week. Relative to the group training once per week, isometric strength gains across the eight joint angles tested were on average twice as large (21.9% vs 10.0%) in the group performing a second set of 8-12 reps at least 48 hours following the first set (52).
It is worth noting that neither of these two studies measured changes in the neck muscle size, so it is unclear how much hypertrophy may have contributed to the increases in strength induced by these very low volumes (37, 52). Nonetheless, two other 12-week resistance training interventions have measured increases in biceps size to occur after performing a single set of 8-12 elbow flexion reps to failure twice per week, so it is certainly plausible that this volume could be sufficient to yield neck muscle hypertrophy as well (9, 59).
Based on the available evidence, performing one set each of neck extension and neck flexion exercise twice per week is a reasonable and time-efficient approach to adding direct neck training into your existing program. As with the pursuit of any other objective, the key to improving neck strength and muscularity is to commit to a plan that can be consistently followed, so it is generally wiser to begin ingraining the habit of neck training with very low volumes which facilitate adherence. A greater rate of initial gains may potentially be experienced if someone starts utilizing higher volumes, but the increased opportunity cost may interfere with neck training consistency for individuals who have a finite amount of training time, which could prompt them to abandon neck training altogether. Once you form the habit with several weeks of minimal-volume neck training, you can incrementally increase set volumes to determine if a higher volume approach enables greater progress.
With respect to rep range selection, I generally encourage beginning with a light to moderately light level of resistance that allows you to perform approximately 15-25 quality reps per set as you refine your neck exercise technique. As employed in three of the discussed resistance training interventions, somewhat heavier 8-12 rep sets can be quite effective for neck training, but the subjects in these studies were directly supervised during their sessions (17, 37, 52). For someone who is independently learning the technique for these exercises without a coach to monitor form, I typically recommend transitioning to moderate loads only after you have consistently demonstrated technical proficiency with lighter resistance.
When performing any of the neck exercise variations where you hold a weight plate against your head, incrementally progressing the load through the addition of smaller diameter light plates can be rather awkward due to how you grip the plates. Particularly when using multiple plates with different diameters, it is difficult to position them properly for neck exercises, so progressing from week to week by increasing reps with a given weight is generally more convenient until you are strong enough to use a heavier single plate for a fairly wide target rep range. For instance, if you start with a 25lb plate for 15-rep sets of neck extension exercise, you can progressively add reps each week with the same weight until you are strong enough to use a 35lb plate for your minimum rep target. This may entail progressing to the point that you can perform 30-rep sets with 25lb before you can utilize 35lb for 15-rep sets. Many lifters will find that this method of progression is more practical than adding 2.5lb and 5lb plates on top of the 25lb plate while using a narrower rep range.
The Relationship Between Neck Strength and Injury
Because head movement occurs through motion at the cervical spine, the muscles which act on the cervical spine serve a pivotal role in stabilizing both the head and neck, which contain the brain and spinal cord comprising the central nervous system. When an external force is applied to the head, individuals with high neck strength tend to experience lower velocity head movement than those with lower neck strength (20). If an athlete’s capacity to stabilize his/her head during a collision is influenced by neck strength, so too may an athlete’s risk of sustaining a concussion be affected by neck strength.
The most notable data on this matter was provided by researchers who measured neck strength and neck circumferences for over 6,000 high school athletes who played soccer, basketball, and lacrosse, while tracking who suffered concussions over the subsequent two years (15). Overall, athletes who later sustained a concussion exhibited significantly lower neck strength and neck circumferences than those who did not experience a concussion during the observation period. These findings suggest that increasing neck muscle strength and size through training may provide a protective effect against concussion risk, although firm conclusions cannot be drawn without longitudinal training interventions. While forceful collisions can occur during soccer, basketball, and lacrosse, I suspect that the overall effect would be even more pronounced in other sports such as hockey, football, boxing, and mixed martial arts where collisions are even more routine. A smaller study examining 27 professional rugby players over the course of two years also sought to assess how neck strength training may affect the risk of suffering a cervical spine injury (45). Relative to the first season when no neck exercise was performed, significantly fewer cervical spine injuries occurred during matches in the second season where the rugby players incorporated a neck strength training program. Despite this favorable finding, the limited sample size restricts the scope of conclusions which may be drawn. To my knowledge, this is the only research that has investigated the potential for neck resistance training by itself to influence a healthy individual’s probability of sustaining an injury. However, rugby players have also experienced a reduced risk of sustaining a concussion or neck injury after participating in other interventions that included neck training along with a variety of different exercises (5,30).
Additionally, individuals suffering from chronic neck pain have experienced significant reductions in pain and disability following neck resistance training interventions (4,8,13). When the available body of evidence is comprehensively analyzed, it is also clear that individuals who experience chronic neck pain typically exhibit lower neck strength than otherwise similar individuals who do not suffer from neck pain (42). Correlation does not equate to causation, so this finding cannot indicate whether neck weakness contributed to the development of neck pain or resulted from pre-existing neck pain. Nonetheless, low neck extensor muscular endurance has been prospectively identified as a risk factor for developing new onset chronic neck pain in office workers with high computer use, so enhancing this quality through training may be beneficial for certain populations (56). While distinct from maximal strength (which was not found to be a risk factor in that study), absolute muscular endurance can be significantly improved through resistance training with a wide loading range, whether that be moderately heavy (e.g., 6-8 RM), moderately light (e.g., 15-20 RM), or light (e.g., 30-40 RM) (60).
Beyond affecting muscle size and strength, direct neck strength training may also influence posture for some individuals. Specifically, neck retraction training interventions have helped alleviate forward head posture, which results from habitually maintaining an excessive degree of upper cervical extension and lower cervical flexion (4,35). It remains to be empirically demonstrated if forward head posture can serve as a contributing factor in the onset of neck pain, but many perceive this posture to be unaesthetic. With its ability to be impacted by a variety of factors including our environment and behavioral habits, posture is a complex phenomenon. Consequently, enhancing the strength and endurance of the neck musculature may not necessarily be sufficient to modify resting head position; however doing so can reduce potential barriers from creating new postural habits.
Neck Retraction with Manual Resistance


Sleep Apnea
Some individuals may be hesitant to perform direct neck exercises out of concern for developing obstructive sleep apnea, which is characterized by repeated bouts of partial or complete restriction of the upper airway while sleeping (3). This highly prevalent disorder, which can reduce blood oxygen concentrations and meaningfully impair sleep quality, is associated with an elevated risk of experiencing multiple diseases (28, 55). Relative to people without obstructive sleep apnea, individuals with this disorder often have greater neck circumferences, and neck circumference is positively correlated with its severity (2, 11, 18, 32, 34, 48). Given this relationship, some lifters may be apprehensive to train their necks with exercises that can increase neck circumference through muscle hypertrophy (63). While neck muscle thickness influences neck circumference, correlation does not equate to causation, and other variables are much more likely to serve a causal role in the development of obstructive sleep apnea.
Neck circumference, waist circumference, body mass index (i.e., weight to height ratio), and body fat percentage all positively correlate with each other (6, 7, 19, 22, 27, 29, 41, 48, 53, 68, 69). While not without exceptions, people in the general population who have rather thick necks will likely be overweight in the same way that people with large waists and high body mass indexes often have high levels of body fat. Neck circumference, waist circumference, and body mass index do not distinguish between lean mass and fat mass, but lifters who have added appreciable amounts of muscle mass are not representative of the average person assessed by these studies. When any of these three variables increase for the typical adult, fat gain is usually the primary reason rather than muscle gain. Like neck circumference, body mass index positively correlates with having obstructive sleep apnea, so it is reasonable to think that obesity may be the root issue rather than neck circumference (11, 51). Nonetheless, neck circumference is associated with obstructive sleep apnea even when controlling for body mass index, suggesting that the location of mass is relevant (34, 61).
Largely due to genetic differences, regional fat distribution varies among individuals, so two individuals with the same level of total body fat may have rather dissimilar fat concentrations at the same anatomical site (10, 40). When lying down to sleep, having a high amount of subcutaneous (i.e., underneath the skin) neck fat may have the potential to compress the upper airway and consequently contribute to obstructive sleep apnea. However, deep fat deposits, which can contribute to a narrowing of the upper airway, are much more likely to be the culprit. Compared to people without obstructive sleep apnea, individuals with this disorder have significantly larger tongues and greater volumes of tongue fat particularly at its base (33, 39, 43, 54). Notably, these differences are present even when adjusting for body mass index and neck circumference (33, 43). Tongue volume positively correlates with body mass index and neck circumference to an even greater degree, so the association that these two variables have with obstructive sleep apnea may in large part be mediated by their relationship with tongue size (26, 36, 46, 57). Of any particular structure, the tongue may be the most relevant with respect to obstructive sleep apnea, but it is not the only contributing variable. Other internal tissues comprising the upper airway are also enlarged with more voluminous fat deposits in individuals with this condition compared to healthy controls with similar body mass indexes (44, 54).
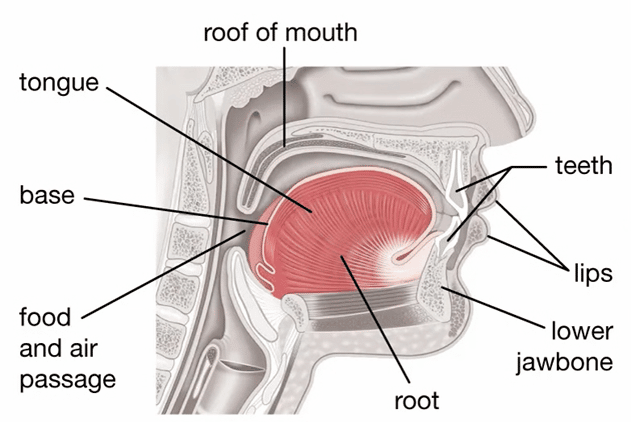
The importance of tongue fat to obstructive sleep apnea is further demonstrated by Wang et al, who examined 67 obese adults with this disorder before and after they completed a weight loss intervention (70). In addition to tracking changes in obstructive sleep apnea severity and bodyweight, the researchers measured a host of anatomical variables including 10 factors relating to upper airway size and 12 soft tissue volume measurements. Congruent with previous findings, the magnitude of weight loss correlated with the degree to which disease severity reduced (23, 58, 66). Intriguingly, the magnitude by which tongue fat volume decreased similarly correlated with reduced obstructive sleep apnea severity and weight loss. When adjusting for participants’ percentage of weight loss, the change in tongue fat volume was the sole variable that significantly correlated with the degree to which obstructive sleep apnea severity decreased. In light of these results, Wang et al concluded that decreases in tongue fat volume serve a primary role in mediating reductions in obstructive sleep apnea severity after weight loss (70).
After reviewing the available body of research, I have yet to see any evidence demonstrating that neck muscle size specifically affects someone’s risk of developing obstructive sleep apnea. This absence of evidence does not necessarily exclude neck muscle size from possibly being a contributing factor for some individuals, but its potential to do so would merely be speculative. Internal fat deposits, particularly those localized at the tongue, are considerably more likely to have a direct impact.
Conclusion
If you wish to increase neck strength for a particular sport or neck muscle size for an aesthetic goal, common back exercises like shrugs, rows, and deadlifts are likely inadequate by themselves. However, you may be able to experience meaningful neck muscle hypertrophy and strength increases through the addition of direct neck exercise into your existing program.
Image Sources
The trapezius, levator scapulae, and cervical vertebrae anatomy images were published by “BodyParts3D, © The Database Center for Life Science,” are licensed as Creative Commons works, and can be found here.
The masticatory and neck muscle anatomy images were published by “OpenStax,” are licensed as a Creative Commons work, and can be found here.
The tongue anatomy image was published by “Encyclopædia Britannica, Inc.” and can be found here.
Sources Cited
- Ackland, DC, Merritt, JS, and Pandy, MG. Moment arms of the human neck muscles in flexion, bending and rotation. Journal of Biomechanics 44: 475–486, 2011.Available from: https://www.sciencedirect.com/science/article/pii/S0021929010005543
- Ahbab, S, Ataoğlu, HE, Tuna, M, Karasulu, L, Çetin, F, Temiz, LÜ, et al. Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome; Evaluation of possible linkage. Med Sci Monit 19: 111–117, 2013.Available from: https://medscimonit.com/abstract/index/idArt/883776
- Al Lawati, NM, Patel, SR, and Ayas, NT. Epidemiology, Risk Factors, and Consequences of Obstructive Sleep Apnea and Short Sleep Duration. Progress in Cardiovascular Diseases 51: 285–293, 2009.Available from: https://www.sciencedirect.com/science/article/pii/S0033062008000765
- Alpayci, M and Ilter, S. Isometric Exercise for the Cervical Extensors Can Help Restore Physiological Lordosis and Reduce Neck Pain: A Randomized Controlled Trial. American Journal of Physical Medicine & Rehabilitation 96: 621–626, 2017.Available from: https://journals.lww.com/ajpmr/Abstract/2017/09000/Isometric_Exercise_for_the_Cervical_Extensors_Can.3.aspx
- Attwood, MJ, Roberts, SP, Trewartha, G, England, ME, and Stokes, KA. Efficacy of a movement control injury prevention programme in adult men’s community rugby union: a cluster randomised controlled trial. Br J Sports Med 52: 368–374, 2018.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5867421/
- Ben-Noun, L, Sohar, E, and Laor, A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res 9: 470–477, 2001.Available from: https://onlinelibrary.wiley.com/doi/full/10.1038/oby.2001.61
- Bochaliya, RK, Sharma, A, Saxena, P, Ramchandani, GD, and Mathur, G. To Evaluate the Association of Neck Circumference with Metabolic Syndrome and Cardiovascular Risk Factors. J Assoc Physicians India 67: 60–62, 2019.Available from: https://europepmc.org/article/med/31304708
- Borisut, S, Vongsirinavarat, M, Vachalathiti, R, and Sakulsriprasert, P. Effects of Strength and Endurance Training of Superficial and Deep Neck Muscles on Muscle Activities and Pain Levels of Females with Chronic Neck Pain. J Phys Ther Sci 25: 1157–1162, 2013.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3818764/
- Bottaro, M, Veloso, J, Wagner, D, and Gentil, P. Resistance training for strength and muscle thickness: Effect of number of sets and muscle group trained. Science & Sports 26: 259–264, 2011.Available from: https://www.sciencedirect.com/science/article/pii/S0765159710001279
- Bouchard, C. Genetic determinants of regional fat distribution. Human Reproduction 12: 1–5, 1997.Available from: https://doi.org/10.1093/humrep/12.suppl_1.1
- Caffo, B, Diener-West, M, Punjabi, NM, and Samet, J. A Novel Approach to Prediction of Mild Obstructive Sleep Disordered Breathing in a Population-Based Sample: The Sleep Heart Health Study. Sleep 33: 1641–1648, 2010.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2982734/
- Cagnie, B, Dickx, N, Peeters, I, Tuytens, J, Achten, E, Cambier, D, et al. The use of functional MRI to evaluate cervical flexor activity during different cervical flexion exercises. Journal of Applied Physiology 104: 230–235, 2008.Available from: https://journals.physiology.org/doi/full/10.1152/japplphysiol.00918.2007
- Chiu, TTW, Lam, T-H, and Hedley, AJ. A Randomized Controlled Trial on the Efficacy of Exercise for Patients With Chronic Neck Pain. Spine 30: E1, 2005.Available from: https://journals.lww.com/spinejournal/Abstract/2005/01010/A_Randomized_Controlled_Trial_on_the_Efficacy_of.27.aspx
- Chung, SH, Her, JG, Ko, T, You, YY, and Lee, JS. Effects of Exercise on Deep Cervical Flexors in Patients with Chronic Neck Pain. Journal of Physical Therapy Science 24: 629–632, 2012.Available from: https://www.jstage.jst.go.jp/article/jpts/24/7/24_629/_article/-char/ja/
- Collins, CL, Fletcher, EN, Fields, SK, Kluchurosky, L, Rohrkemper, MK, Comstock, RD, et al. Neck Strength: A Protective Factor Reducing Risk for Concussion in High School Sports. J Primary Prevent 35: 309–319, 2014.Available from: https://doi.org/10.1007/s10935-014-0355-2
- Conley, MS, Meyer, RA, Bloomberg, jacob J, Feeback, DL, and Dudley, GA. Noninvasive Analysis of Human Neck Muscle Function. Spine 20: 2505–2512, 1995.Available from: https://journals.lww.com/spinejournal/Abstract/1995/12000/Noninvasive_Analysis_of_Human_Neck_Muscle.9.aspx
- Conley, MS, Stone, MH, Nimmons, M, and Dudley, GA. Specificity of resistance training responses in neck muscle size and strength. Eur J Appl Physiol 75: 443–448, 1997.Available from: https://doi.org/10.1007/s004210050186
- Davies, RJ and Stradling. The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. European Respiratory Journal 3: 509–514, 1990.Available from: https://erj.ersjournals.com/content/3/5/509
- Deurenberg, P, Andreoli, A, Borg, P, Kukkonen-Harjula, K, de Lorenzo, A, van Marken Lichtenbelt, WD, et al. The validity of predicted body fat percentage from body mass index and from impedance in samples of five European populations. Eur J Clin Nutr 55: 973–979, 2001.Available from: https://www.nature.com/articles/1601254
- Eckner, JT, Oh, YK, Joshi, MS, Richardson, JK, and Ashton-Miller, JA. Effect of Neck Muscle Strength and Anticipatory Cervical Muscle Activation on the Kinematic Response of the Head to Impulsive Loads. Am J Sports Med 42: 566–576, 2014.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4344320/
- Elliott, JM, O’Leary, SP, Cagnie, B, Durbridge, G, Danneels, L, and Jull, G. Craniocervical Orientation Affects Muscle Activation When Exercising the Cervical Extensors in Healthy Subjects. Archives of Physical Medicine and Rehabilitation 91: 1418–1422, 2010.Available from: https://www.sciencedirect.com/science/article/pii/S0003999310003102
- Flegal, KM, Shepherd, JA, Looker, AC, Graubard, BI, Borrud, LG, Ogden, CL, et al. Comparisons of percentage body fat, body mass index, waist circumference, and waist-stature ratio in adults. The American Journal of Clinical Nutrition 89: 500–508, 2009.Available from: https://doi.org/10.3945/ajcn.2008.26847
- Foster, GD, Borradaile, KE, Sanders, MH, Millman, R, Zammit, G, Newman, AB, et al. A Randomized Study on the Effect of Weight Loss on Obstructive Sleep Apnea Among Obese Patients With Type 2 Diabetes: The Sleep AHEAD Study. Archives of Internal Medicine 169: 1619–1626, 2009.Available from: https://doi.org/10.1001/archinternmed.2009.266
- Franco, JL and Herzog, A. A Comparative Assessment of Neck Muscle Strength and Vertebral Stability. Journal of Orthopaedic & Sports Physical Therapy 8: 351–356, 1987.Available from: https://www.jospt.org/doi/abs/10.2519/jospt.1987.8.7.351
- Gao, Y, Kristensen, LA, Grøndberg, TS, Murray, M, Sjøgaard, G, and Søgaard, K. Electromyographic Evaluation of Specific Elastic Band Exercises Targeting Neck and Shoulder Muscle Activation. Applied Sciences 10: 756, 2020.Available from: https://www.mdpi.com/2076-3417/10/3/756
- Genta, PR, Schorr, F, Eckert, DJ, Gebrim, E, Kayamori, F, Moriya, HT, et al. Upper Airway Collapsibility is Associated with Obesity and Hyoid Position. Sleep 37: 1673–1678, 2014.Available from: https://doi.org/10.5665/sleep.4078
- Gonçalves, VSS, Faria, ERD, Franceschini, SDCC, and Priore, SE. Neck circumference as predictor of excess body fat and cardiovascular risk factors in adolescents. Rev Nutr 27: 161–171, 2014.Available from: http://www.scielo.br/j/rn/a/rKQkHDnHD6sv9GKW4PDd37h/?lang=en
- Gottlieb, DJ and Punjabi, NM. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 323: 1389–1400, 2020.Available from: https://doi.org/10.1001/jama.2020.3514
- Hingorjo, MR, Qureshi, MA, and Mehdi, A. Neck circumference as a useful marker of obesity: a comparison with body mass index and waist circumference. J Pak Med Assoc 62: 36–40, 2012.Available from: https://jpma.org.pk/article-details/3224?article_id=3224
- Hislop, MD, Stokes, KA, Williams, S, McKay, CD, England, ME, Kemp, SPT, et al. Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial. Br J Sports Med 51: 1140–1146, 2017.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5530334/
- Javanshir, K, Amiri, M, Mohseni Bandpei, MA, De las Penas, CF, and Rezasoltani, A. The effect of different exercise programs on cervical flexor muscles dimensions in patients with chronic neck pain. J Back Musculoskelet Rehabil 28: 833–840, 2015.Available from: https://content.iospress.com/articles/journal-of-back-and-musculoskeletal-rehabilitation/bmr593
- Kawaguchi, Y, Fukumoto, S, Inaba, M, Koyama, H, Shoji, T, Shoji, S, et al. Different Impacts of Neck Circumference and Visceral Obesity on the Severity of Obstructive Sleep Apnea Syndrome. Obesity 19: 276–282, 2011.Available from: https://onlinelibrary.wiley.com/doi/abs/10.1038/oby.2010.170
- Kim, AM, Keenan, BT, Jackson, N, Chan, EL, Staley, B, Poptani, H, et al. Tongue Fat and its Relationship to Obstructive Sleep Apnea. Sleep 37: 1639–1648, 2014.Available from: https://doi.org/10.5665/sleep.4072
- Kim, SE, Park, BS, Park, SH, Shin, KJ, Ha, SY, Park, J, et al. Predictors for Presence and Severity of Obstructive Sleep Apnea in Snoring Patients: Significance of Neck Circumference. J Sleep Med 12: 34–38, 2015.Available from: http://www.e-jsm.org/journal/view.php?year=2015&vol=12&spage=34
- Kong, Y-S, Kim, Y-M, and Shim, J. The effect of modified cervical exercise on smartphone users with forward head posture. J Phys Ther Sci 29: 328–331, 2017.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5332998/
- Lee, RWW, Sutherland, K, Chan, ASL, Zeng, B, Grunstein, RR, Darendeliler, MA, et al. Relationship Between Surface Facial Dimensions and Upper Airway Structures in Obstructive Sleep Apnea. Sleep 33: 1249–1254, 2010.Available from: https://doi.org/10.1093/sleep/33.9.1249
- Leggett, SH, Graves, JE, Pollock, ML, Shank, M, Carpenter, DM, Holmes, B, et al. Quantitative assessment and training of isometric cervical extension strength. Am J Sports Med 19: 653–659, 1991.Available from: https://doi.org/10.1177/036354659101900618
- Li, F, Laville, A, Bonneau, D, Laporte, S, and Skalli, W. Study on cervical muscle volume by means of three-dimensional reconstruction. Journal of Magnetic Resonance Imaging 39: 1411–1416, 2014.Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/jmri.24326
- Lowe, AA, Fleetham, JA, Adachi, S, and Ryan, CF. Cephalometric and computed tomographic predictors of obstructive sleep apnea severity. American Journal of Orthodontics and Dentofacial Orthopedics 107: 589–595, 1995.Available from: https://www.sciencedirect.com/science/article/pii/S088954069570101X
- Malis, C, Rasmussen, EL, Poulsen, P, Petersen, I, Christensen, K, Beck-Nielsen, H, et al. Total and Regional Fat Distribution is Strongly Influenced by Genetic Factors in Young and Elderly Twins. Obesity Research 13: 2139–2145, 2005.Available from: https://onlinelibrary.wiley.com/doi/abs/10.1038/oby.2005.265
- Mendes, CG, Barbalho, SM, Tofano, RJ, Lopes, G, Quesada, KR, Detregiachi, CRP, et al. Is Neck Circumference As Reliable As Waist Circumference for Determining Metabolic Syndrome? Metabolic Syndrome and Related Disorders 19: 32–38, 2021.Available from: https://www.liebertpub.com/doi/abs/10.1089/met.2020.0083
- Miranda, IF, Wagner Neto, ES, Dhein, W, Brodt, GA, and Loss, JF. Individuals With Chronic Neck Pain Have Lower Neck Strength Than Healthy Controls: A Systematic Review With Meta-Analysis. Journal of Manipulative and Physiological Therapeutics 42: 608–622, 2019.Available from: https://www.sciencedirect.com/science/article/pii/S0161475418303257
- Mohan Lal, B, Vyas, S, Malhotra, A, Ray, A, Gupta, G, Pandey, S, et al. Ultrasonography of the neck in patients with obstructive sleep apnea. Sleep Breath , 2022.Available from: https://doi.org/10.1007/s11325-022-02682-3
- Mortimore, IL, Marshall, I, Wraith, PK, Sellar, RJ, and Douglas, NJ. Neck and Total Body Fat Deposition in Nonobese and Obese Patients with Sleep Apnea Compared with That in Control Subjects. Am J Respir Crit Care Med 157: 280–283, 1998.Available from: https://www.atsjournals.org/doi/full/10.1164/ajrccm.157.1.9703018
- Naish, R, Burnett, A, Burrows, S, Andrews, W, and Appleby, B. Can a Specific Neck Strengthening Program Decrease Cervical Spine Injuries in a Men’s Professional Rugby Union Team? A Retrospective Analysis. J Sports Sci Med 12: 542–550, 2013.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3772600/
- Nashi, N, Kang, S, Barkdull, GC, Lucas, J, and Davidson, TM. Lingual Fat at Autopsy. The Laryngoscope 117: 1467–1473, 2007.Available from: https://onlinelibrary.wiley.com/doi/abs/10.1097/MLG.0b013e318068b566
- Oi, N, Pandy, M, Myers, B, Nightingale, R, and Chancey, V. Variation of neck muscle strength along the human cervical spine. Stapp car crash journal 48: 397–417, 2004.Available from: https://pubmed.ncbi.nlm.nih.gov/17230275/
- Onat, A, Hergenç, G, Yüksel, H, Can, G, Ayhan, E, Kaya, Z, et al. Neck circumference as a measure of central obesity: Associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clinical Nutrition 28: 46–51, 2009.Available from: https://www.sciencedirect.com/science/article/pii/S0261561408001933
- Ordway, NR, Seymour, RJ, Donelson, RG, Hojnowski, LS, and Edwards, WT. Cervical flexion, extension, protrusion, and retraction. A radiographic segmental analysis. Spine (Phila Pa 1976) 24: 240–247, 1999.Available from: https://journals.lww.com/spinejournal/Abstract/1999/02010/Cervical_Flexion,_Extension,_Protrusion,_and.8.aspx
- Panjabi, MM and White, AA. Basic biomechanics of the spine. Neurosurgery 7: 76–93, 1980.Available from: https://pubmed.ncbi.nlm.nih.gov/7413053/
- Peppard, PE, Young, T, Barnet, JH, Palta, M, Hagen, EW, and Hla, KM. Increased Prevalence of Sleep-Disordered Breathing in Adults. American Journal of Epidemiology 177: 1006–1014, 2013.Available from: https://doi.org/10.1093/aje/kws342
- Pollock, ML, Graves, JE, Bamman, MM, Leggett, SH, Carpenter, DM, Carr, C, et al. Frequency and volume of resistance training: Effect on cervical extension strength. Archives of Physical Medicine and Rehabilitation 74: 1080–1086, 1993.Available from: https://www.sciencedirect.com/science/article/pii/000399939390065I
- Qureshi, NK, Hossain, T, Hassan, MI, Akter, N, Rahman, MM, Sultana, MM, et al. Neck Circumference as a Marker of Overweight and Obesity and Cutoff Values for Bangladeshi Adults. Indian J Endocrinol Metab 21: 803–808, 2017.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5729663/
- Schwab, RJ, Pasirstein, M, Pierson, R, Mackley, A, Hachadoorian, R, Arens, R, et al. Identification of Upper Airway Anatomic Risk Factors for Obstructive Sleep Apnea with Volumetric Magnetic Resonance Imaging. Am J Respir Crit Care Med 168: 522–530, 2003.Available from: https://www.atsjournals.org/doi/full/10.1164/rccm.200208-866OC
- Senaratna, CV, Perret, JL, Lodge, CJ, Lowe, AJ, Campbell, BE, Matheson, MC, et al. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Medicine Reviews 34: 70–81, 2017.Available from: https://www.sciencedirect.com/science/article/pii/S1087079216300648
- Shahidi, B, Curran-Everett, D, and Maluf, KS. Psychosocial, Physical, and Neurophysiological Risk Factors for Chronic Neck Pain: A Prospective Inception Cohort Study. The Journal of Pain 16: 1288–1299, 2015.Available from: https://www.sciencedirect.com/science/article/pii/S1526590015008676
- Shigeta, Y, Ogawa, T, Ando, E, Clark, GT, and Enciso, R. Influence of tongue/mandible volume ratio on oropharyngeal airway in Japanese male patients with obstructive sleep apnea. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 111: 239–243, 2011.Available from: https://www.oooojournal.net/article/S1079-2104(10)00801-2/fulltext
- Smith, PL, Gold, AR, Meyers, DA, Haponik, EF, and Bleecker, ER. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med 103: 850–855, 1985.Available from: https://pubmed.ncbi.nlm.nih.gov/3933396/
- Sooneste, H, Tanimoto, M, Kakigi, R, Saga, N, and Katamoto, S. Effects of Training Volume on Strength and Hypertrophy in Young Men. The Journal of Strength & Conditioning Research 27: 8–13, 2013.Available from: https://journals.lww.com/nsca-jscr/FullText/2013/01000/Effects_of_Training_Volume_on_Strength_and.2.aspx
- Stone, WJ and Coulter, SP. Strength/Endurance Effects From Three Resistance Training Protocols With Women. The Journal of Strength & Conditioning Research 8: 231–234, 1994.Available from: https://journals.lww.com/nsca-jscr/abstract/1994/11000/strength_endurance_effects_from_three_resistance.5.aspx
- Stradling, JR and Crosby, JH. Predictors and prevalence of obstructive sleep apnoea and snoring in 1001 middle aged men. Thorax 46: 85–90, 1991.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC462949/
- Suderman, BL and Vasavada, AN. Neck Muscle Moment Arms Obtained In-Vivo from MRI: Effect of Curved and Straight Modeled Paths. Ann Biomed Eng 45: 2009–2024, 2017.Available from: https://doi.org/10.1007/s10439-017-1830-8
- Taylor, MK, Hodgdon, JA, Griswold, L, Miller, A, Roberts, DE, and Escamilla, RF. Cervical Resistance Training: Effects on Isometric and Dynamic Strength. Aviation, Space, and Environmental Medicine 77: 1131–1135, 2006.Available from: https://pubmed.ncbi.nlm.nih.gov/17086765/
- Thompson, DJ, Throckmorton, GS, and Buschang, PH. The effects of isometric exercise on maximum voluntary bite forces and jaw muscle strength and endurance. Journal of Oral Rehabilitation 28: 909–917, 2001.Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2842.2001.00772.x
- Tsang, SM, Chan, KT, Ho, PL, Kwok, JC, Tse, DH, and Tsoi, HH. Comparison between velocity‐specific exercise and isometric exercise on neck muscle functions and performance: a randomised clinical trial. BMC Musculoskeletal Disorders 22: 81, 2021.Available from: https://doi.org/10.1186/s12891-021-03943-0
- Tuomilehto, HPI, Seppä, JM, Partinen, MM, Peltonen, M, Gylling, H, Tuomilehto, JOI, et al. Lifestyle Intervention with Weight Reduction. Am J Respir Crit Care Med 179: 320–327, 2009.Available from: https://www.atsjournals.org/doi/10.1164/rccm.200805-669OC
- Vasavada, AN, Li, S, and Delp, SL. Influence of Muscle Morphometry and Moment Arms on the Moment-Generating Capacity of Human Neck Muscles. Spine 23: 412–422, 1998.Available from: https://journals.lww.com/spinejournal/Abstract/1998/02150/Influence_of_Muscle_Morphometry_and_Moment_Arms_on.2.aspx
- Verma, M, Rajput, M, Sahoo, SS, and Kaur, N. Neck Circumference: Independent Predictor for Overweight and Obesity in Adult Population. Indian J Community Med 42: 209–213, 2017.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5682719/
- Wang, C, Hou, X-H, Zhang, M-L, Bao, Y-Q, Zou, Y-H, Zhong, W-H, et al. Comparison of Body Mass Index with Body Fat Percentage in the Evaluation of Obesity in Chinese. Biomedical and Environmental Sciences 23: 173–179, 2010.Available from: https://www.sciencedirect.com/science/article/pii/S0895398810600499
- Wang, SH, Keenan, BT, Wiemken, A, Zang, Y, Staley, B, Sarwer, DB, et al. Effect of Weight Loss on Upper Airway Anatomy and the Apnea–Hypopnea Index. The Importance of Tongue Fat. Am J Respir Crit Care Med 201: 718–727, 2020.Available from: https://www.atsjournals.org/doi/full/10.1164/rccm.201903-0692OC




